Yeast infections can affect various body parts but most commonly affect the mouth and genitals. There are different types of yeast infections, which can occur in acute or chronic forms. Candidiasis can produce various symptoms, depending on the area of the body occupied by the fungi. Yeast infection is often associated with skin symptoms. Proper diagnosis of candidiasis is crucial to begin treatment. If left untreated, candidiasis can lead to a systemic body infection. Learn about methods of diagnosing and treating fungal infections.
Risk Factors
Different types of Candida fungi can cause infections in humans. In healthy individuals, Candida fungi colonize the mucous membranes of the gastrointestinal tract. Candida infection is opportunistic, meaning that the fungi cause infections under specific conditions. The most common situation involves a lowered immune system, resulting in fungal pathogenicity. Risk factors, therefore, include:
- Diseases
- Antibiotic therapy
- Diet
- Age
- Pregnancy
Diseases
Prevailing diseases and inflammatory conditions are associated with weakened immunity, predisposing to yeast infection. Some diseases increase this risk due to their characteristics. It has been noted that candidiasis is more common in people with diabetes. In diabetics, the mucous membranes’ epithelial cells are more susceptible to yeast adhesion and growth.
In addition, oral candidiasis is a common condition in HIV-infected people. This virus type is associated with weakened immunity and exposure to various infections, not just fungi. Other predisposing factors for candidiasis include tuberculosis, hypoparathyroidism, Addison’s disease, and many others.
Antibiotic Therapy
Candidiasis is often associated with antibiotic therapy. Antibiotics and immunosuppressants are a major predisposing factor in the increased incidence of fungal infections. Taking antibiotics can, among other things, alter the pH of the vagina, destroying lactic acid bacilli and creating an environment ideal for fungal proliferation. Antibiotics taken in excessive amounts over a long time can cause side effects. Sometimes, it also takes a toll on dental health and overall oral health.
Antibiotic treatment that lasts too long and the associated decrease in immunity can lead to the proliferation of pathogens and oral infections too quickly. Chemotherapies can also cause an increased risk of yeast infection. Cancer cytotoxic chemotherapy can cause a disease caused by Candida albicans.

Diet
Risk factors also include nutritional deficiencies. Nutrients such as vitamins A, B6, and iron are essential. Sometimes, vitamin deficiencies contribute to the development of ringworm. In a study conducted, it was noted that taking vitamin A helped inhibit yeast growth. Also, B vitamins block Candida growth enzymes. Also, adequate levels of iron in the body play an important role in preventing Candida albicans infection. Iron is essential for maintaining the body’s immunity.
Thus, an adequate diet rich in nutrients is vital for candida infections. It’s also worth noting that eating a diet high in sugars can increase the possibility of getting Candida. Probiotics, which support the state of the intestinal microflora, are also essential ingredients.
Age
As we age, the rate of candidiasis increases. Among other things, seniors have a higher incidence of oral infections caused by Candida albicans. Candidiasis is a reasonably common problem, especially in people over 60. Seniors are at higher risk of yeast infection due to comorbidities and reduced immunity.
In addition, infants are also in the risk group for candidiasis. Candidiasis in infants is most often a Candida infection in the oral mucosa. Candidiasis in newborns also occurs due to contact with a fungus in a woman’s reproductive tract. This yeast occurs there naturally and can infect the baby during natural childbirth.
Pregnancy
Pregnant women are vulnerable to fungal infections. The risk of yeast infection is most significant at the beginning of pregnancy, when the female body produces enormous amounts of hormones and the economy is severely disrupted. The natural protective barrier is weakened, and pathogenic microorganisms multiply more quickly.
Intimate infections are common ailments during pregnancy. They require treatment because they can be dangerous to the unborn child. Untreated vaginal fungal infections in pregnancy can result in premature labor and even miscarriage. Also, it is common for pathogens to be transmitted from mother to child during childbirth.

Types
Many types of Candida are listed; one common species is C. albicans. Candida albicans is a fungus that is a natural component of human bacterial flora, and under favorable conditions leads to infection. Candidiasis can be divided not only by the type of fungus but also by the area occupied. Fungi can affect the mouth, vagina, penis, or other parts of the body.
Candidiasis can cause many symptoms, from mild to acute infections. Yeast infections can also take chronic forms. In some cases, disseminated candidiasis is most often associated with acquired or hereditary immune deficiencies. Superficial candidiasis, on the other hand, is the most common form.
Oral Candidiasis
Oral yeast infection can occur as various entities. The condition includes multiple forms, including hyperplastic candidiasis, atrophic candidiasis, pseudomembranous candidiasis, erythema of the gums, tongue inflammation, and lips inflammation. Fungal infection of the oral cavity is commonly referred to as thrush. Symptoms include:
- White patches
- Painful swallowing
White Patches
Oral thrush infection primarily manifests as white spots on the tongue, throat, and other mouth areas. White, soft, and slightly raised plaques are most common on the tongue and cheek walls—the mucosal lesions consist of tangled masses of fungal filaments admixed with exfoliated epithelium and bacteria. The white plaque, when wiped away, leaves an erythematous area. The pseudomembranous form is common in chronically ill patients and infants. In contrast, hyperplastic candidiasis, also known as yeast-induced leukoplakia, has precancerous potential.

Swallowing Pain
Oral candidiasis can cause additional symptoms related to soreness and difficulty swallowing. In addition, there may be burning and dryness in the throat, painful cracking at the corners of the mouth, and bad breath. However, these symptoms do not necessarily accompany an oral infection, the most common symptom being mucosal lesions. In mild infections, painful symptoms are not intense or not present at all.
Vaginal Candidiasis
Infection of the vagina and vulva with Candida yeast is called yeast infection. The infection can affect the vagina, vaginal entrance, and labia. The disease occurs when too much yeast builds up on the mucous membranes, which causes inflammation in large clusters. At certain stages of life, women are more prone to yeast infection. In some cases, the infection is asymptomatic. However, vaginal candidiasis can cause the following symptoms:
- Discomfort
- Redness
- Abnormal vaginal discharge
Discomfort
Vaginal candidiasis can cause several unpleasant discomforts. There may be burning and itching in the vagina or vulva area. This makes sexual intercourse painful. The unpleasant burning sensation can cause significant discomfort and pain, affecting quality of life. In addition, the infection can also affect the urethra, causing pain during urination. Symptoms of vaginal candidiasis can worsen a few days before the onset of menstruation. Men also have candidiasis of the genital area, which a man can contract from an affected partner. Men often have asymptomatic infections.

Redness
Inflammation can be detected by noticing redness in the mucous membranes of the vagina or vulva. The inflamed membranes become red and are covered with a whitish coating. The inflammation can spread to the external genitals. Then, areas such as the labia may also become red and swollen.
Abnormal Vaginal Discharge
Vaginal candidiasis can cause abnormal discharge with specific characteristics. Women with a yeast infection may notice a whitish-yellowish vaginal discharge. The discharge can vary in density, mostly thick and cottage cheese-like, while it can also be watery. White vaginal discharge may be secreted in large quantities during candida inflammation.
Systemic Candidiasis
Untreated yeast infection can affect other body parts and lead to systemic disease. Systemic candidiasis can also occur in newborns infected from the mother during birth. The risk of infection is increased with prematurity and low birth weight. Developed systemic candidiasis is dangerous because it can lead to sepsis.
Systemic candidiasis can also be challenging to diagnose because it produces uncharacteristic symptoms such as fever, chills, and hypotension. The symptoms of the disease also depend on the organ involved. Systemic candidiasis can affect various organs and systems. If you suspect candidiasis, see a doctor who, based on your symptoms and general condition, will guide the diagnosis and prescribe treatment.

Diagnosis
Candida are fungi that produce spores within two hours after entering the human body. Fungi of this type reproduce at 37 degrees Celsius. When Candida is present in the human body, it can be detected through tests. However, the first diagnostic step is usually a history and analysis of the symptoms of candidiasis.
In women, a gynecological examination is performed. Gynecologists must distinguish fungal infections from bacterial infections of the vagina and vulva to introduce appropriate treatment. White plaque is easy to recognize and usually indicates a fungal infection. However, laboratory tests are needed to demonstrate the specific type of Candida fungus.
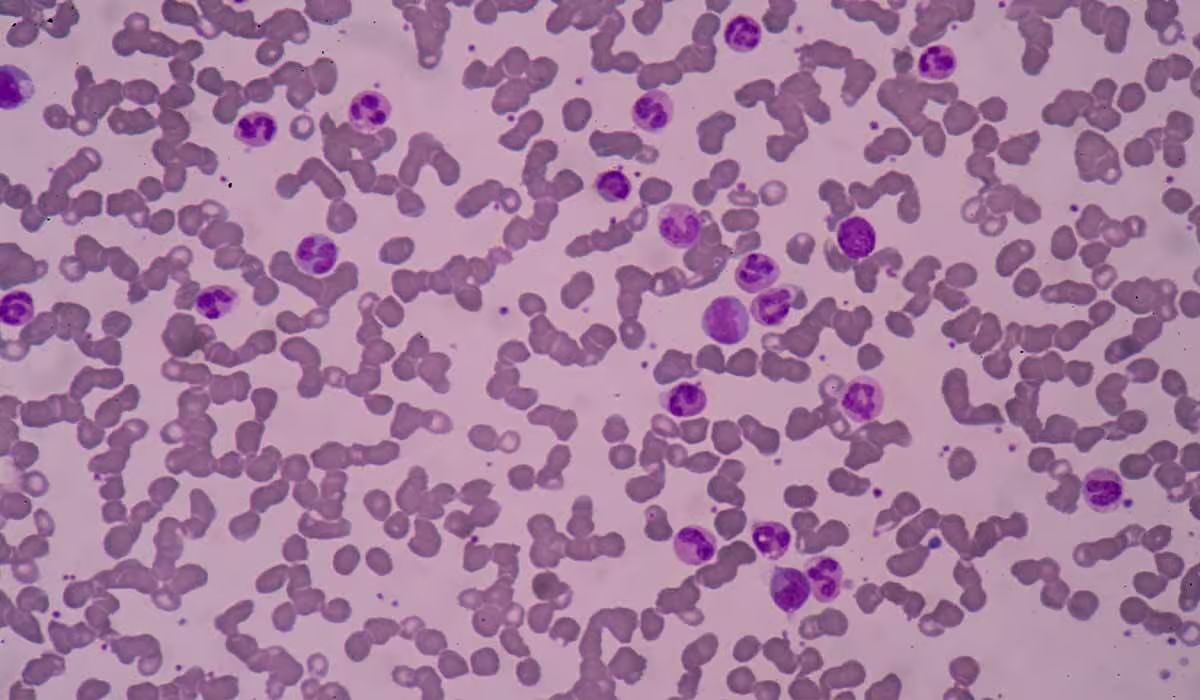
Laboratory Tests
A sample of secretions from mucous membranes occupied by the fungus can be analyzed in detail. Examination under a microscope or performing a fungal culture in the laboratory will indicate specific strains of Candida. Doctors can see budding yeast under a microscope. On the other hand, for rare systemic candidiasis, blood cultures are performed.

Treatment
Once a fungal infection is disseminated correctly, the treatment process can begin. Treatment of yeast infections is essential to avoid complications and the spread of pathogens to other parts of the body. Different treatment methods are used depending on the area occupied by Candida fungi. Generally, antifungal drugs in various forms are used.
Antifungal Drugs
Fungal infections are treated with particular substances that destroy the fungi. Oral or vaginal medications are used, depending on the case and severity of the infection. Doctors usually prescribe antifungal drugs such as clotrimazole, nystatin, and miconazole. For mild genital Candida infections, an antifungal cream applied to the affected mucous membranes may suffice. Lozenges are also used for oral candidiasis.
Treatment time can vary, with treatment lasting from 1 to 7 days. In case of systemic candidiasis or severe course, treatment may be more prolonged. Topical and oral therapies have similar high efficacy. It is also worth remembering that treatment may cause burning or itching as a side effect. If you have a vaginal infection, you may also need to treat your partner.
Probiotics
Oral use of probiotics can serve as an adjunct in the treatment of oral or vaginal candidiasis. It is possible to use capsules containing lactic acid bacteria, which restores the balance in the vagina and supports the healing process. Probiotics can also be used orally. Probiotic supplementation for several weeks has proven effective in eliminating symptoms of vaginal candidiasis. It is also good to compensate for vitamin and iron deficiencies and follow a low-sugar diet during treatment.
Summary
Yeast infection is associated with Candida fungi, which colonize different body areas. Many risk factors influence the onset of a yeast infection. These include a weakened immune system and antibiotic therapy. Pregnant women are also at risk of Candida infection due to hormonal changes. A yeast infection can produce different symptoms depending on the affected area.
Vaginal candidiasis is associated with discomfort and symptoms in the vaginal and vulvar areas. The severe form of candidiasis is systemic, which leads to serious complications. However, local yeast infections are common and amenable to antifungal treatment. Diagnosis of yeast infections is based on laboratory tests.
Sources
- Arya N. R, Naureen B. Rafiq (2023). Candidiasis.
https://www.ncbi.nlm.nih.gov/books/NBK560624/ - Institute for Quality and Efficiency in Health Care (2022). Overview: Vaginal yeast infection (thrush).
https://www.ncbi.nlm.nih.gov/books/NBK543220/ - Zahra Vahedpoor, Mahdi Abastabar, Mojtaba Sehat, Parisa Talebian, Tayebeh Felfelian Fini, Zahra Dastanpour, Iman Haghani, Ramtin Chelongarian, Mehdi Nazeri (2021). Vaginal and oral use of probiotics as adjunctive therapy in patients with vulvovaginal candidiasis: A clinical trial on Iranian women.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9006731/