Central and peripheral vertigo are distinguished depending on where the cause of vertigo is located.
Peripheral vertigo is dizziness caused by a peripheral cause, i.e., outside the central nervous system. These include:
- Inner ear injury (fracture of the pyramid of the temporal bone, perilymphatic fistula, labyrinth concussion)
- Labyrinthitis
- Inner ear cancer
- Labyrinth ischemia
- Meniere’s Syndrome
- Labyrinthine otosclerosis
- Motion sickness
Central vertigo is dizziness that is caused by the major nervous system conditions. These include:
- Strokes, e.g., of the brainstem and cerebellum
- Brain tumors
- Multiple sclerosis
- Migraine
- Epileptic seizure
- Head injuries
- Illness or infection
Symptoms
The main symptom is a feeling of movement or spinning, which may result in nausea and vomiting.
Visual disturbances (scotoma), headache, impaired consciousness, convulsions, and paresis of limbs or cranial nerves may accompany them.
In the peripheral type, the patient has the impression of circular movements. They start suddenly, are very intense, especially at the beginning, become weaker over time, last from several dozen minutes to several hours, and head movements intensify them. They may be accompanied by hearing disorders (hearing loss, deafness, tinnitus, feeling of fullness in the ear) and, very rarely, headaches.

Diagnosis
If you experience vertigo, consult your doctor. The specialist should start a visit with a medical interview. Its goal is to determine whether the patient’s sensations indicate systemic or non-systemic vertigo. The doctor may ask whether the patient feels:
- Precise illusion of movement (usually circular, rotation of the environment or one’s own body or head in space), the so-called peripheral vertigo (most often associated with the peripheral part of the balance system).
- The imprecise illusion of instability, the uncertainty of posture, lack of balance or fear of falling, and so-called dizziness (related to the central part of the balance system).
- Not dizzy symptoms – a feeling of lightheadedness, fainting (presyncope) accompanied by vegetative symptoms, and tachycardia – most often accompany systemic diseases or mental disorders (e.g., panic disorder).
It is also crucial to determine the characteristics of vertigo over time:
- How long has the vertigo been present
- Is vertigo permanent or appear often
The specialist will also ask whether there are other symptoms coexisting with vertigo and under what circumstances this condition occurs:
- Short-lasting attacks of systemic vertigo occurring in specific, constant positions for a given patient, e.g., going to bed, standing up, dizziness to the side, bending over, etc. (benign positional vertigo).
- Dizziness following tinnitus and a feeling of fullness in the ear (Meniere’s syndrome).
- They are spinning vertigo without hearing impairment, nausea, vomiting, and significant severity of symptoms (vestibular neuritis, viral labyrinthitis).
- Vertigo is accompanied by damage to the cranial nerves or sensory disturbances – usually hernia or ataxia (stroke, brain tumor).
- Consciousness disorders (tumor, meningitis, ischemic or hemorrhagic stroke, poisoning).
- Headache (the nature of the pain is significant; the differentiation should include both migraine, in which we expect the incidents to be stereotypical, and a possible stroke).
- Recurrent dizziness followed by a headache may suggest vestibular migraine (difficulty in diagnosis is the fact that, according to some authors, in some cases, the headache does not appear at all).
- Psychiatric symptoms (anxiety, depression, etc.).
The patient will be asked whether there were factors preceding the onset of symptoms:
- Infection
- Past head injury
- The relationship between symptoms and physical exercise
- Manual therapy of the cervical spine, more extended flexion position
It is significant to talk about overall health, especially about the risk of vascular disease:
- Comorbidities – arterial hypertension (pressure fluctuations, anxiety control); diabetes (episodes of hypoglycemia); heart diseases (cardiac arrhythmias, low ejection fraction, heart failure); endocrine disorders (hypothyroidism); mental illnesses.
The doctor usually also asks about family medical history, taking prescriptions (remember that vertigo may result from side effects of medications), or using stimulants (e.g., alcohol or caffeine).
Tests for diagnosing vertigo include, e.g.:
- The Fukuda-Unterberger test – a doctor may ask you to march in place with your eyes closed for 30 seconds. If you rotate or lean to one side, it could indicate an issue with your inner ear labyrinth, which may result in vertigo.
- Romberg’s test – during this procedure, a specialist will ask you to stand with your feet together, close your eyes, and keep your arms at your side. Feelings of unsteadiness or imbalance may happen due to an issue with your central nervous system, which contains your brain and spinal cord.
- Head Impulse Test – the doctor will move your head from side to side. During this procedure, you must concentrate your vision on an unmoving target. This test can detect whether the issues are in the balance system in your inner ear.
- Vestibular Test Battery – various tests can help to review the vestibular portion of your inner ear system. A vestibular test battery may determine if your symptoms stem from an inner ear or brain issue.
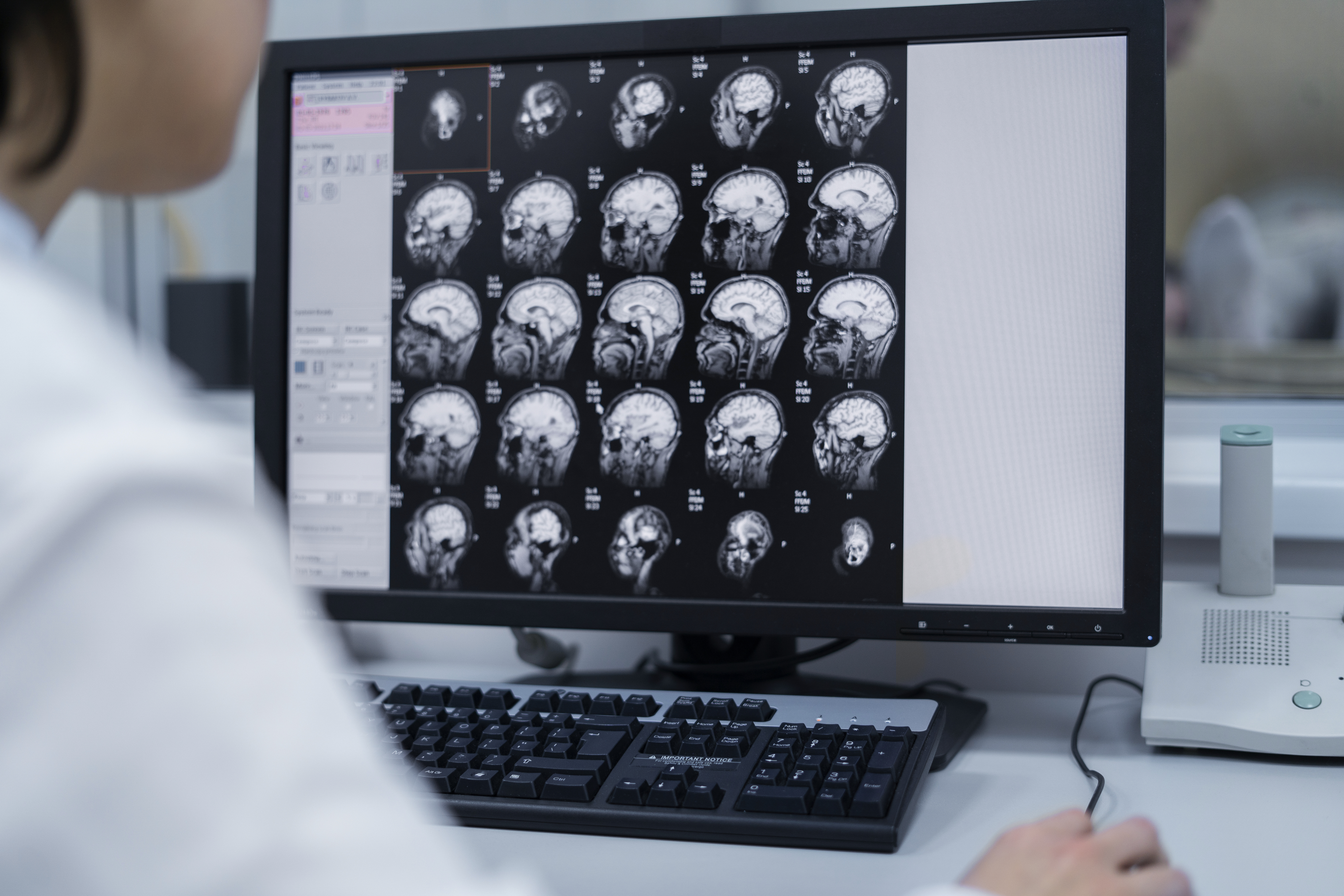
At this stage, the specific cause of the disease can already be recognized. To make it more precise, you can additionally perform, depending on the need, e.g.:
- Imaging tests (these include computed tomography and magnetic resonance of the head),
- Electroencephalography,
- Carotid artery ultrasound,
- Caloric tests (allowing detection of a problem with the labyrinth),
- Electronystagmography (used to assess nystagmus accurately),
- Heart ECG examination,
- Laboratory tests (lipidogram, diabetic curve, thyroid hormones, etc.).
Treatment
Therapy for vertigo depends on the cause of this condition. In many circumstances, it goes away without any treatment. It is because the brain can adjust, at least partially, to the inner ear modifications, depending on additional mechanisms to maintain balance.
Central compensation is the primary goal of vestibular rehabilitation. It should be used as early as possible. It effectively controls persistent dizziness resulting from damage to the peripheral part of the vestibular system, both in unilateral and bilateral dysfunction cases.
Drug therapy is warranted if dizziness persists for several hours to several days. On the one hand, in shorter-term dizziness, drugs usually have no effect, and on the other hand, prolonged therapy impairs the central mechanisms for compensating vestibular functions, which are the most effective in combating dizziness.
In everyday practice, in the acute phase of symptoms, antihistamine and antiemetic drugs are used (in most patients, drugs of choice), and if there is no effect, sedative drugs (benzodiazepines). Sedatives are not recommended for treating vertigo unless the symptoms are severe. Medications should be used for the shortest possible time and discontinued when the symptoms can be controlled without pharmacotherapy. This approach enables the activation of compensatory mechanisms.
In some circumstances, surgery may be fundamental to treating vertigo. If the underlying cause of the condition is a severe problem like a tumor or brain or neck injury, managing those problems could reduce the vertigo symptoms.
Home Remedies
In case of any ailments, it is always worth using natural and safe ways to alleviate them first. They are available almost immediately.
First of all, when vertigo appears:
- Rest
- Sit down and stand up slowly when the dizziness subsides
- Move slowly and carefully
- Do not bend down suddenly
- Do not get up suddenly after sitting/lying
- Do not ignore the feeling of dizziness
- Do not do anything dangerous while feeling dizzy (e.g., driving, climbing ladders, operating machinery, etc.)
- If dizziness and other symptoms persist, consult the specialist
Below are other helpful tips.
The Epley Maneuver
One technique is The Epley Maneuver. It is also called canalith repositioning. This method uses head and body movements to remove crystals from inner ear canals.
The person lies on their back for 2 minutes with their head tilted back off the couch and turned 45° towards the affected ear, then turns 90° towards the healthy ear. This results in the otoliths’ displacement to the semicircular canal’s mouth. Then, they rotate their head another 90° towards the healthy ear and tilt it down. The individual stays in this position for about 2 minutes. Then, they return to the sitting position, which causes the otoliths to move into the vestibule.
Do Not Forget About Physical Activity
Exercise is an antidote to many diseases. It not only improves coordination and balance but also blood circulation. Thanks to this, the body is better nourished and oxygenated. Regular activity not only has a positive impact on your well-being but also effectively reduces dizziness.
Sleep is the Best Medicine For Every Ailment
If you have trouble falling asleep, do not force yourself to fall asleep. You should go to bed and stay in bed only if you feel drowsy. Do not force yourself to fall asleep earlier than usual.
Other than sleeping everyday activities should also be separated from the bedroom. Watches should also be removed from the bedroom or placed so that they are not visible or accessible from the bed. If you can’t help but want to know what time it is at night, you can always check it in another room.
It is better not to perform emotionally or physically arousing activities in the evening. If you have to work longer in the evening or have experienced something unpleasant, you should delay going to bed.
In the evening, it is also recommended to wear loose clothes, 1-2 hours before going to bed, it is worth taking a warm bath, after which you should do pleasant activities, for example listening to relaxing music.

Choose Relaxation Methods
Relaxation means reduced muscle tension, general body mobilization, and inner peace. There are many relaxation techniques.
Biofeedback is a therapeutic method that involves learning to control changes in physiological activity. A particular machine is used for it. Data regarding the patient’s biological activity is continuously collected, processed, and provided in the form of feedback (visual or acoustic), thanks to which the individual can modify this activity. Presenting information about changes in body function allows us to direct attention to these processes to influence their course, even if they are usually unconscious. The flow path of this information creates a closed loop. Two phenomena are responsible for the psychophysiological effect of biofeedback therapy: psychological–instrumental conditioning and neurophysiological–neuroplasticity of the nervous system.
One of them is visualization. It involves actively creating multi-sensory images and feeling the accompanying emotions. Images are the mental representation of an absent object or event. The direct purpose of their use is to induce a specific change depending on the content of the image being created. The essence of visualization training is to use imagination in such a way as to properly “program” the mind to change actions or thought patterns, which leads to increased adaptation and development possibilities.
Acupressure
This method stimulates specific anatomical points on the skin surface by puncturing thin metal needles, which can be produced manually or electrically. The effect of acupuncture depends on stimulation and involves activating the body’s neuroendocrine response with the involvement of peripheral and central mechanisms.
Sources
- Physiology, Vestibular System. NIH. https://www.ncbi.nlm.nih.gov/books/NBK532978/.
- Vertigo. NIH. https://www.ncbi.nlm.nih.gov/books/NBK482356/.
- Peripheral Vertigo. NIH. https://www.ncbi.nlm.nih.gov/books/NBK430797/.
- Vertigo: A Review of Common Peripheral and Central Vestibular Disorders. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3096243/.
- Central Vertigo. NIH. https://www.ncbi.nlm.nih.gov/books/NBK441861/.
- Benign Paroxysmal Positional Vertigo. NIH. https://www.ncbi.nlm.nih.gov/books/NBK470308/.
- Vertigo and Associated Symptoms. NIH. https://www.ncbi.nlm.nih.gov/books/NBK228/.
- Diagnosis and Treatment of Vertigo and Dizziness. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2696792/#s2title.
- The assessment of fukuda stepping test results in prognosis of benign paroxysmal postural vertigo. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9734258/.
- Romberg Test. NIH. https://www.ncbi.nlm.nih.gov/books/NBK563187/.
- Evaluation of video head impulse test during vertiginous attack in vestibular migraine. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9330756/.
- Test Batteries and the Diagnostic Algorithm for Chronic Vestibular Syndromes. NIH. https://pubmed.ncbi.nlm.nih.gov/34867755/.
- Vestibular Rehabilitation. NIH. https://www.ncbi.nlm.nih.gov/books/NBK572153/.
- Surgical treatment of vertigo. NIH. https://pubmed.ncbi.nlm.nih.gov/8178103/.
- Epley Maneuver. NIH. https://www.ncbi.nlm.nih.gov/books/NBK563287/.
- Efficacy and safety of acupuncture for dizziness and vertigo in emergency department: a pilot cohort study. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4459064/.
- Physical Activity in the Prevention of Benign Paroxysmal Positional Vertigo: Probable Association. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4296996/.
- Vestibular vertigo is associated with abnormal sleep duration. NIH. https://pubmed.ncbi.nlm.nih.gov/29064831/.
- Guided Visualization: Dealing with Stress. NIH. https://www.nimh.nih.gov/news/media/2021/guided-visualization-dealing-with-stress.
- Is Biofeedback for Vertigo Effective in Ordinary Medical Centers? A Controlled Trial in Northern Italy. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10412656/.