For example, Candida albicans occur in 40-80 percent of healthy people and belongs to the physiological flora of the digestive tract. Candida fungi can also occur in the membrane of the respiratory system or the membrane of the urinary system. Since these fungi are naturally present in our bodies, it is worth noting that yeast infection is a disease that develops only in favorable conditions for the microorganism to multiply.
Causes
The proliferation of yeasts of the genus Candida occurs due to damaged immune system functioning and disturbance of the balance in the composition of the microflora of the human body. Factorsthat may contribute to this include:
- Long-term antibiotic therapy – antibiotics destroy beneficial bacterial flora, which inhibits the development of fungi.
- Hormonal contraception – can contribute to the development of vaginal yeast infection. Hormones, which are the main component of contraceptive pills, reduce the population of Lactobacillus bacteria, which are responsible for maintaining a low pH in the vagina. The decrease in the number of bacteria increases the pH, which allows the fungus to multiply excessively.
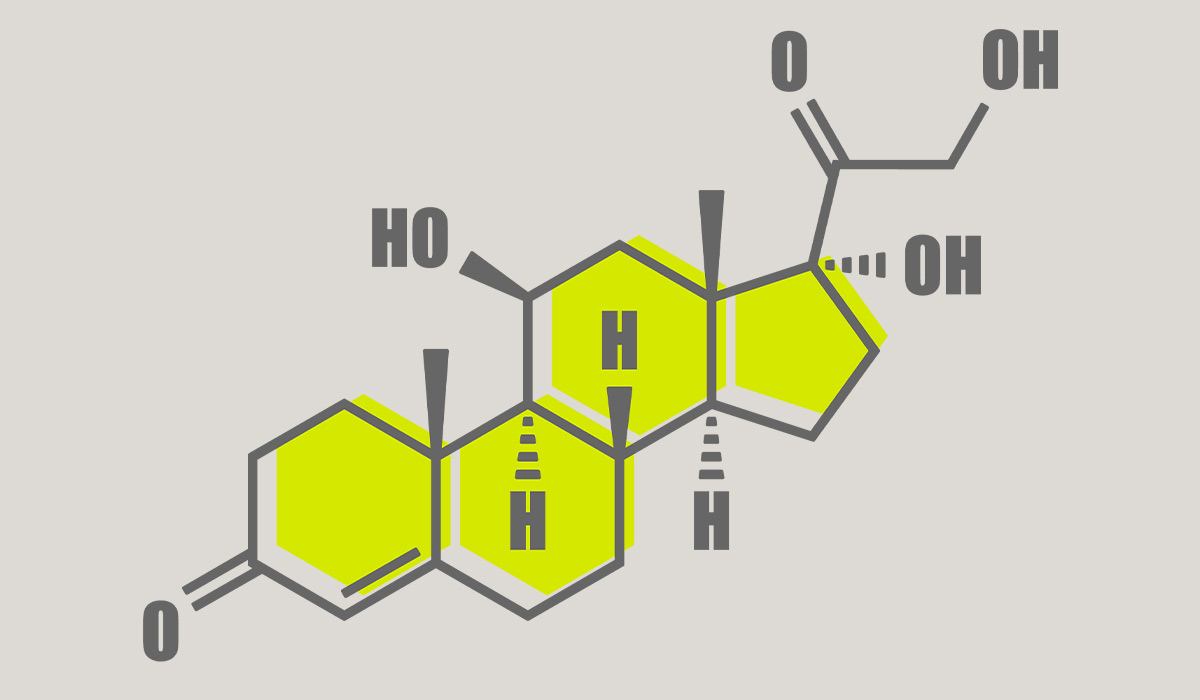
- Increased estrogen levels – yeast infections are more prevalent in people who have higher estrogen levels — such as pregnant women or the ones taking high-dose estrogen birth control pills or other estrogen hormone treatment (like replacement therapy).
- Chemotherapy – as a result of chemotherapy, cancer cells and healthy cells of the organism are destroyed, including epithelial cells that are a barrier protecting against excessive colonization of the body by fungi. Chemotherapy also negatively affects immune mechanisms.
- Weakened immunity – can be caused by numerous disease conditions, including primary and secondary immune disorders (like HIV), surgery, extensive burns, and injuries (for example, epithelial damage).
Other risk factors include:
- Excessive sweating,
- Diabetes,
- Obesity,
- Pregnancy and childbirth,
- Alcoholism,
- Drug addiction,
- Endocrine disorders,
- Use of steroids,
- Malabsorption syndrome,
- Eating disorders,
- Blood diseases,
- Other contraceptive use includes vaginal sponges, diaphragms, and intrauterine devices (IUDs).
Moreover, yeast infection happens due to improper hygiene (for example douching or hygiene neglect), and in very humid and warm conditions. The disease may also be caused by direct contact with a person infected with the Candida fungus.

Types and Symptoms
Yeast infection can take many forms. There are three main types of infections: generalized superficial and systemic infections.
Generalized candidiasis develops mainly in immunosuppressed people – it’s a state of reduced immunity, which gives the possibility of excessive development and spread of Candida. Such situations occur especially in the case of insufficient immunity of cells, which is becoming more common due to the development of medicine. The weakening of the immune system is quite common in people after organ transplants (in their case, the immunity is deliberately lowered so that the body does not reject the transplanted organ). The state of weakened immunity also occurs in patients struggling with AIDS and people taking immunosuppressive drugs in the course of autoimmune disease treatment.
The weakening of the immune system is also a problem for oncology patients receiving chemotherapy (a side effect of chemotherapy is neutropenia, i.e., a reduction in the number of neutrophils, which are important cells involved in defense against infections).
Weakened immunity is also a problem for people addicted to drugs and alcohol, people with eating disorders (bulimia, anorexia), malnourished people, and patients with deficiencies of B vitamins. It’s worth noticing that candidiasis is transmitted through the circulatory system, but it can involve various organs and tissues. For this reason, people who are immunocompromised are advised to be cautious.
Superficial candidiasis can affect various parts of the skin, appendages, and mucous membranes, while systemic candidiasis influences one organ in our body (an example can be fungal endocarditis). Superficial candidiasis can also attack us due to generalized infection with the dominance of symptoms from one organ. Depending on the stage of candidiasis, appropriate medications are prescribed for patients. It is necessary to use antifungal creams or ointments, nail polishes, mouthwashes, and some oral medications.
Symptoms
If you start to experience intense itching of the vagina and its surroundings, your body is likely struggling with a yeast infection. The diagnosis is almost inevitable if a white, caseous discharge accompanies it. Do not underestimate this ailment to prevent the development of the disease, inflammation, and dangerous complications. Be sure to contact a gynecologist who will prescribe the appropriate treatment.
In addition to smooth skin, thrush can affect mucous membranes, such as the vulva or the penis. Quite often symptoms you may experience if you develop a genital yeast infection include:
- Thick white discharge (like cottage cheese),
- An unpleasant smell,
- Different degrees of inflammation,
- Burning and itching sensation (especially while urinating or during sex),
- Splits in the genital skin,
- Difficulty pulling back the foreskin.
The main risk factors are pregnancy, diabetes, and obesity, as well as poor personal hygiene and contact with infected people. The severity of symptoms ranges from slight itching and burning to painful swelling. Ignoring these yeast infection symptoms can lead to more severe health problems (like urethritis).
In men, the infection mainly affects the foreskin and the glans of the penis, while in women mainly the vagina and the vulva. Then, there is tenderness in the organs affected by the infection and pain during urination and sex. Patients may also notice whitish spots and ulcers with whitish discharges of dense consistency during the disease. The disease may be accompanied by itching and burning.
The more developed the vaginal candidiasis is, the more troublesome the symptoms caused by vaginal yeast will be. Vaginal itching will intensify, and inflammation and associated burning will appear, especially when urinating.

Penis Mycosis – Male Yeast Infection
Although intimate fungal infections are considered to be typically female, it should be remembered that thrush can also affect men. Normally, mycosis of the penis develops after intercourse with an infected person or during antibiotic therapy. In the initial stage, penile thrush is usually asymptomatic, after some time a man may notice redness around the glans of the penis, a white coating under the foreskin, and he begins to feel pain that intensifies during urination and ejaculation.
To avoid intimate infections, not only vaginal thrush, you should take care of proper hygiene of the intimate area (liquids and emulsions for cleaning intimate places will be helpful). In addition, to support the maintenance of the physiological vaginal microbiome, it is worth using gynecological probiotics. However, when candidiasis develops, you should consult a doctor and introduce antifungal drugs.
Diagnosis
The diagnosis is mainly based on medical history, symptoms, pelvic exam, and microscopic examination of a vaginal smear. It is also helpful to perform a vaginal biocenosis test. Sometimes, we deal with infections of mixed etiology (bacterial and fungal). That said, a microbiological test of a smear from the genital tract is used to make the proper diagnosis.

How Is It Treated?
Symptoms will not go away on their own. Vaginal thrush is a disease and, like any disease, requires treatment tailored to its stage of development. Abandonment of therapy recommended by a specialist or its arbitrary discontinuation may lead to health-threatening complications.
Candidiasis can become a chronic disease and begin to attack not only the vulva area but also other parts of the female reproductive system, including the cervix and fallopian tubes. Ultimately, it can lead to infertility. But that’s not all! Yeast can also begin to invade other organs outside of the genital system. Curing such an advanced disease is a big challenge for specialists.
The basic principles of candida treatment are focused on:
- The correct selection of the drug to which Candida yeasts are sensitive;
- Selection of the least toxic drug and the most appropriate drug depending on comorbidities, such as renal failure, liver damage, etc.;
- The appropriate duration of treatment;
- Continuation of treatment despite the resolution of symptoms;
- Proper hygiene of the affected sites is important in case of superficial mycosis.
Among the drugs for intimate infections that a gynecologist may recommend, there are primarily antibiotics. It is also beneficial to use topical ointments for vaginal mycosis. The most common is clotrimazole.
Medications for intimate infections will bring the fastest results if treatment starts early enough. The more advanced the candidiasis, the longer the therapy usually takes to restore normal vaginal microflora. The treatment of recurrent vaginal thrush is particularly complicated. If the disease develops at least four times a year, supplementing it with clotrimazole may be necessary. Most yeast infections clear up within a few days, but the duration of treatment depends on many factors, including the severity of the disease and recommended medication.
Home remedies for yeast infection will not bring the expected results. The help of a specialist – a dermatologist, a venereologist, or a gynecologist, who will conduct a thorough examination and prescribe appropriate medications is necessary. The topic should not be underestimated and ignored because the disease tends to spread spontaneously and recur.
An excellent idea for supporting the treatment and preventing the recurrence of yeast infections is the use of gynecological probiotics. They contain specially selected live bacterial cultures that help rebuild the bacterial flora of the vagina. Probiotics are available in two forms – vaginal and oral.
The vaginal probiotic works well in situations where strong and fast action is required because it is applied topically. This form is often chosen for antibiotic therapy or treatment of an intimate infection. Oral probiotics are absorbed from the digestive tract, delaying its action. It is mainly used when it is necessary to act preventively or when applying a topical probiotic is impossible, for example, due to irritation or a previous procedure.
It is also recommended to avoid sexual intercourse while having intimate infections. This action will prevent the spreading of disease from an infected person. Sexual abstinence will also help speed up healing.
Prevention
The effectiveness of mycosis treatment depends on several factors – following the rules of proper therapy allows for optimal treatment results. There is no one effective way to prevent vaginal yeast infection. Implementing a few simple habits, however, can reduce the likelihood of disease recurrence. As mentioned above, it is worth taking gynecological probiotics because they help to maintain the physiological balance of the vaginal microflora. The intimate areas should not be cleaned more than twice a day, preferably with plain water or with special products such as mild liquids and emulsions for cleaning the intimate areas. To prevent the risk of developing a yeast infection, it is recommended to use only personal toiletries.
You can also try home remedies to prevent infection, like solutions with herbal extracts of aloe, sage, nettle, or marigold (however, home remedies should not be considered a treatment). It is also worth wearing comfortable and airy underwear, which helps avoid sweating, moisture accumulation, and abrasions.
It is also beneficial to avoid skin contact with constantly moist objects and sexual contact with potentially ill people. Moreover, getting screened regularly for high-risk factors is always recommended to prevent the development of severe diseases and take care of overall health.
Sources
- Vaginal Candidiasis. Centers for Disease Control and Prevention. July 13, 2022.
https://www.cdc.gov/fungal/diseases/candidiasis/genital/index.html - Yeast Infection. Jefferson Health.
https://www.jeffersonhealth.org/conditions-and-treatments/yeast-infection - Vaginal Yeast Infections. U.S. Department of Health and Human Services Office on Women’s Health. February 22, 2021.
https://www.womenshealth.gov/a-z-topics/vaginal-yeast-infections - Vulvovaginal Candidiasis (VVC). Centers for Disease Control and Prevention. July 22, 2021.
https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm - Lindberg S. Can You Have Sex With a Yeast Infection? Self. February 12, 2022.
https://www.self.com/story/yeast-infection-sex