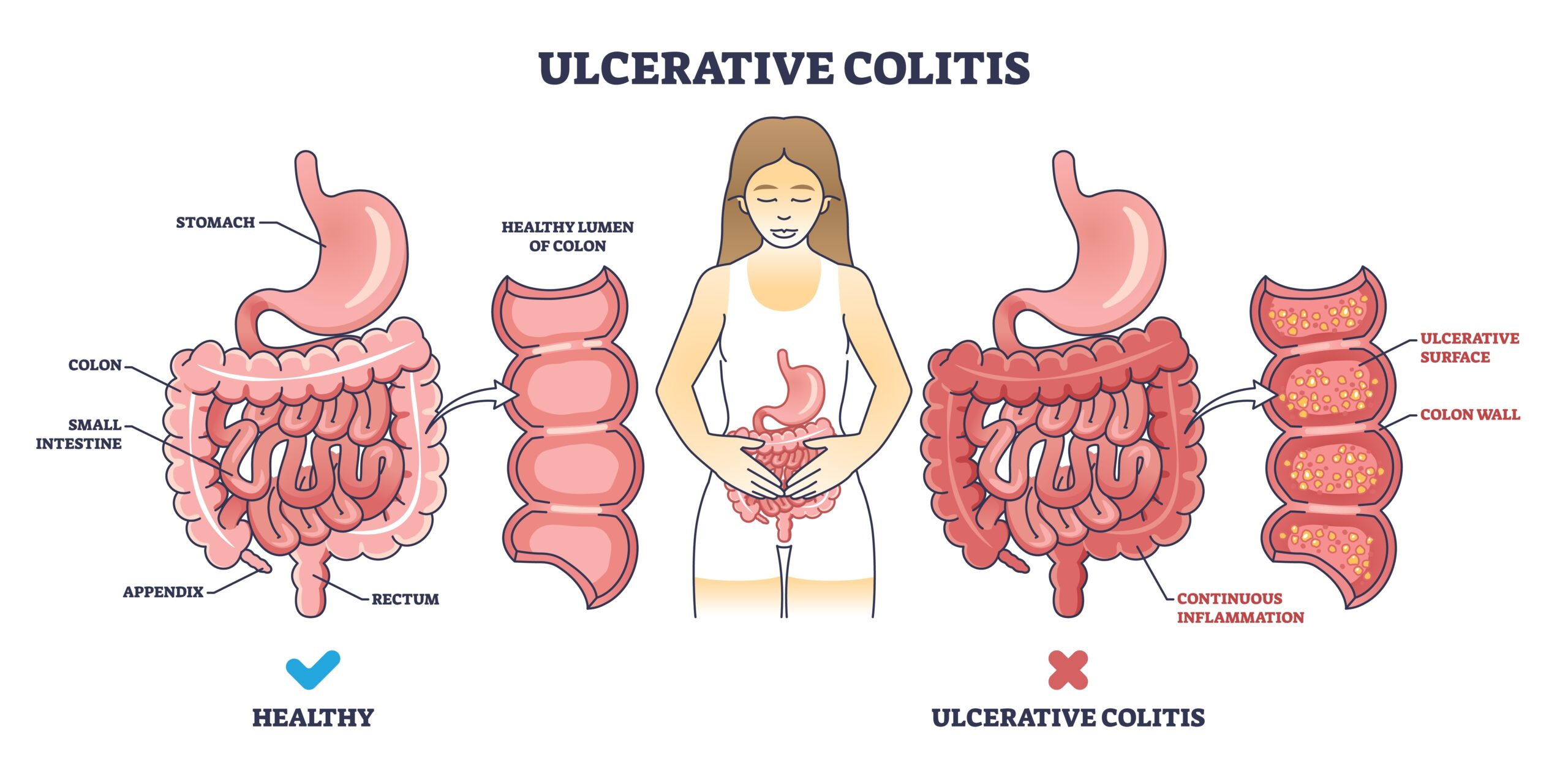
Ulcerative colitis (UC) is one of the inflammatory bowel diseases (IBD). IBD is a group of conditions that affect the digestive tract. Inflammation in the colon or rectum leads to ulcerative colitis. In some cases, inflammation of both organs may occur.
The inflammation leads to the formation of small ulcers on the colon’s inner surface. Typically, these sores originate in the rectum and spread upwards, affecting the entire colon.
Inflammation results in the death of cells on the colon lining, giving rise to ulcers. They, in turn, cause bleeding and secretion of mucus and pus in the feces.
Ulcerative colitis affects people of all ages, with most patients diagnosed between 15 and 30. After age 50, there is another slight increase in the diagnosis of this disease, usually in men. Studies show that it affects up to 600 000 adults in the US.
Ulcerative colitis can have a substantial impact on life quality and can sometimes lead to life-threatening complications. Getting the right treatment for this condition can greatly reduce the symptoms of the disease and even result in long-lasting improvement

Causes
The exact causes of ulcerative colitis are unknown. However, we know that the development of the disease is favored by:
- genetic predisposition (it often runs in families)
- diet
- intestinal infections
- abnormal composition of gut bacterial flora
However, the most significant importance is attributed to the malfunctioning of the immune system. It reacts to factors that are indifferent to a healthy body for unknown reasons. This excessive immune response triggers an uncontrolled inflammatory process that leads to damage to the colon wall, bleeding ulcers, and stiffening of the walls with flattening of the intestinal folds.
Symptoms
In the course of ulcerative colitis, the following are often observed:
- Diarrhea, often bloody, is the dominant symptom. The stool can be passed very often but with a small volume, which is the result of inflammatory changes in the rectum
- abdominal pain (usually in the lower abdomen on the left side or in the rectum)
- fever
- weakness
- weight loss
If only the rectum is involved, bloody diarrhea may occur, accompanied by a strong urge to defecate, pain, and loss of bowel control.
Most patients with ulcerative colitis have a mild course of the disease. In this case, the only symptoms may be diarrhea and bleeding. In the benign course of the illness, stools are passed less than four times a day.
Moderately severe disease is characterized by up to 6 bloody stools per day, abdominal pain, abdominal tenderness, fever, and weakness.
Severe course manifests itself by:
- passing more than six bloody stools a day
- significant weakness
- fever
- increased heart rate
- lowering blood pressure
- abdominal pain

Impact of ulcerative colitis on other organs
Joints
Ulcerative colitis can cause problems outside of the intestines. Joint problems such as swelling and pain (arthritis) affect about one in 10 people with UC.
The elbows, wrists, knees, and ankles are most commonly affected, but the spine and pelvic joints can also be affected. Joint problems can come and go. For some people, joint problems will worsen during a flare-up, but in others, it can occur even without bowel symptoms.
Skin
Colitis can also cause skin problems. An erythema nodosum affects up to 10% of people with UC. The inflammation causes painful, reddish lumps that typically appear on the legs and develop into bruises. This condition usually occurs during flare-ups and resolves with the treatment of colitis.
Eyes
Some people with colitis develop eye inflammation. The eye condition most often associated with UC is called episcleritis, an inflammation of the layer covering the whites of the eye. This causes redness, soreness, and inflammation. Episcleritis has a tendency to worsen at the same time as colitis and may need medication to reduce inflammation.
Inflammation of the iris and the white of the eye, called uveitis and scleritis respectively, have been associated with colitis. If these conditions are not treated, they can cause a loss of vision.
Blood
Individuals with colitis can be more likely to have anemia (a medical state in which there are not enough red blood cells). This is due to the absorption issues caused by the intestinal inflammation. Iron is necessary for red blood cell production, so if there is not enough of it in the body, red blood cell production is impaired.
People with UC are also more likely to develop blood clots in the veins, including deep vein thrombosis (DVT) in the legs. The likelihood of experiencing it is greater during an outbreak of symptoms or when lying in bed, such as in a hospital.
Bones
Individuals with colitis may have a greater risk of having bones that are fragile and thin, which might be caused by:
- the inflammation process
- difficulty in absorbing the calcium needed for the production of bones
- low calcium levels since some people with UC might avoid dairy products (a natural source of calcium)
- the use of certain medications.
Diagnosis
To diagnose ulcerative colitis, the doctor performs an examination and asks about symptoms. Then, the doctor performs additional tests to confirm the diagnosis and differentiate the disease from other diseases with similar symptoms.
Endoscopy (sigmoidoscopy, colonoscopy)
The test that allows to establish the final diagnosis and assess the extent of changes is endoscopy of the large intestine with the collection of specimens for microscopic examination. During the disease, inflammatory changes begin in the rectum and continuously extend toward the remaining sections of the large intestine.
CT (Computed Tomography), X-ray, Ultrasound
These methods help the doctor to recognize changes outside the bowel and complications caused by ulcerative colitis.
Treatment
The goal of treatment is to heal the mucosa, which means to subside the inflammatory changes. Treatment is modified depending on disease activity (relapses). When an episode of illness is occurring, more rigorous treatment is applied than in periods of stability (while undergoing maintenance therapy). The goal of maintenance therapy is to prevent relapses. Avoiding stress, gastrointestinal infections, oral antibiotics, and non-steroidal anti-inflammatory drugs is essential during maintenance therapy.
Medicines used in therapy mainly have anti-inflammatory properties. Some medications are designed to reduce the activity of the immune system, and in exacerbations of the disease, antibiotics and other modern medicines that effectively reduce inflammation are used.
Surgery is sometimes necessary, especially when exacerbations are frequent and severe. Surgery used in people with ulcerative colitis involves the removal of the large intestine and is called a colectomy.
After such an operation, defecation is possible through one of the following options:
- Ileostomy involves making a surgical hole in the abdominal wall and exposing a small intestine fragment to the abdomen’s surface. In this case, the waste is discharged into a pouch (bag) connected to the stoma.
- Creating a connection between the small intestine and the anus, an ileoanal anastomosis (also known as a J-pouch) is performed. In this case, feces are excreted through the anus.
Diet for ulcerative colitis
People with ulcerative colitis may need to change their diet to relieve their symptoms. No diet or meal plan is suitable for everyone with ulcerative colitis, and diets are individualized for each person. Depending on the symptoms, different types of diets are recommended, such as:
- Low-fat diet – Eating fatty foods can trigger symptoms in people with UC. Doctors often suggest a diet that includes limited amounts of fat, usually during times of increased symptoms of ulcerative colitis.
- A low-residue diet involves eating foods that contain very minimal amounts of fiber, so the body produces less waste and the person has fewer bowel movements.
- Gluten-free diet: people with ulcerative colitis may be sensitive to gluten.
It is of utmost importance for those suffering from ulcerative colitis to be aware of their nutritional intake since episodes of diarrhea and bleeding can lead to dehydration and an imbalance of electrolytes, vitamins, and minerals. You may need to take dietary supplements if your symptoms do not allow you to follow a nutritionally balanced diet.
Complications
Bowel cancer
People with inflammatory bowel disease have a higher chance of developing bowel cancer. Factors that increase the risk of its occurrence include the long duration of the disease and the involvement of a large part of the large intestine. As time progresses, the chance of getting cancer increases.
Because the symptoms of bowel cancer resemble those of UC (abdominal pain, diarrhea, blood in stool), it can be easily overlooked – individuals with ulcerative colitis are monitored cautiously for colon cancer.
Check-ups for bowel cancer in people with UC involve colonoscopy, an examination during which the doctor inserts a tube with a camera through the anus into the large intestine. The doctor carefully examines the inside of the intestines on the monitor, looking for any abnormalities, and if found, collects small samples for microscope examination.
This type of check-up is carried out for people with the disease every 1-5 years, depending on the duration of the disease (the longer the person is ill, the more frequent examinations are necessary).
Osteoporosis
Osteoporosis causes bones to become weaker and susceptible to breaking. People with ulcerative colitis have a higher chance of developing this condition due to:
- Ulcerative colitis can cause problems with food absorption and, thus, deficiency of substances needed to keep bones healthy.
- Some medications used in UC treatment can cause osteoporosis.
If this issue arises, the physician will advise taking vitamin D and calcium to strengthen the bones.
Toxic megacolon
Toxic megacolon is a condition that causes the large intestine to become dilated and distended. If this occurs, the colon cannot pass gasses from the body, leaving it stuck in the intestines. This is a severe condition that can be life-threatening. It can lead to a hole (perforation) in the intestine or infection spreading to the blood (sepsis).
Symptoms of the disease may appear suddenly and include:
- severe general condition
- stomachache
- high fever
- tachycardia (heart beating too fast)
Treatment of toxic megacolon includes antibiotics, fluids, and steroids. Sometimes, when the condition doesn’t improve after medications, surgery involving the removal of the large intestine (colectomy) is necessary.
Primary sclerosis cholangitis
Primary sclerosis cholangitis (PSC) is a condition that some people with UC may develop. This disease affects the bile ducts, which are destroyed due to inflammation.
Primary sclerosis cholangitis usually shows symptoms when the disease is already advanced. PSC symptoms are similar to ulcerative colitis, so it is not difficult to overlook this condition in people with UC. These symptoms include:
- tiredness
- diarrhea
- jaundice (yellowing of the skin and whites of the eyes)
- skin itching
- weight loss
- fever
There is no specific treatment for PSC. Medications are used to relieve symptoms. Sometimes a liver transplant is necessary when the disease is very advanced.
Is it possible to completely cure ulcerative colitis?
Treatment of ulcerative colitis is chronic and consists in preventing relapses and alleviating the course of exacerbations. A complete cure is probably impossible, but there are mild forms of the disease without exacerbations.
The only case when ulcerative colitis is completely cured and does not return is a surgical treatment involving the removal of the entire large intestine (colectomy).
How are ulcerative colitis and Crohn’s disease different?
Ulcerative colitis and Crohn’s disease are chronic inflammatory bowel disease types. However, there are critical distinctions between them. Both diseases cause digestive system inflammation, but different areas of the gut are affected.
Similarities between ulcerative colitis and Crohn’s disease include:
- both disorders often develop in young adults
- there is no distinction between genders in terms of whom these diseases affect
- the symptoms of each are similar
- The reasons behind UC and Crohn’s disease remain a mystery, and both conditions have similar factors that increase the chances of getting them, including environmental, genetic, and abnormal reactions by the body’s immune system.
Ulcerative colitis and Crohn’s disease differences include:
- Ulcerative colitis is restricted to the large intestine, whereas Crohn’s disease can affect any area from the mouth to the rectum.
- Crohn’s disease involves healthy parts of the intestine coming between segments of inflammation, while ulcerative colitis is simply a widespread inflammation of the large intestine.
- UC involves only the innermost layer of the colon, while Crohn’s disease can potentially affect all the intestines’ different layers.
When should you see a doctor?
In case of bleeding from the gastrointestinal tract, recurrent diarrhea, abdominal pain, fever, or unintentional weight loss, you should contact your GP for proper tests.
People who have been diagnosed with ulcerative colitis and have an exacerbation of symptoms of the disease should immediately report to a doctor who will decide on the need for hospital treatment or continuation of therapy on an outpatient basis.
Sources
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Ulcerative Colitis (2020) https://www.niddk.nih.gov/health-information/digestive-diseases/ulcerative-colitis
- Kappelman MD, Moore KR, Allen JK, Cook SF. Recent trends in the prevalence of Crohn’s disease and ulcerative colitis in a commercially insured US population. Dig Dis Sci. 2013 Feb;58(2):519-25. doi: 10.1007/s10620-012-2371-5. Epub 2012 Aug 29. PMID: 22926499; PMCID: PMC3576554. https://pubmed.ncbi.nlm.nih.gov/22926499/
- Weaver KN, Herfarth H. Gluten-Free Diet in IBD: Time for a Recommendation? Mol Nutr Food Res. 2021 Mar;65(5):e1901274. doi: 10.1002/mnfr.201901274. Epub 2020 Jun 28. PMID: 32558265. https://pubmed.ncbi.nlm.nih.gov/32558265/
- Fritsch J, Garces L, Quintero MA, Pignac-Kobinger J, Santander AM, Fernández I, Ban YJ, Kwon D, Phillips MC, Knight K, Mao Q, Santaolalla R, Chen XS, Maruthamuthu M, Solis N, Damas OM, Kerman DH, Deshpande AR, Lewis JE, Chen C, Abreu MT. Low-Fat, High-Fiber Diet Reduces Markers of Inflammation and Dysbiosis and Improves Quality of Life in Patients With Ulcerative Colitis. Clin Gastroenterol Hepatol. 2021 Jun;19(6):1189-1199.e30. doi: 10.1016/j.cgh.2020.05.026. Epub 2020 May 20. PMID: 32445952. https://pubmed.ncbi.nlm.nih.gov/32445952/
- National Health Service (NHS) Living with Ulcerative colitis (2022) https://www.nhs.uk/conditions/ulcerative-colitis/living-with/
- Orchard TR. Management of arthritis in patients with inflammatory bowel disease. Gastroenterol Hepatol (N Y). 2012 May;8(5):327-9. PMID: 22933865; PMCID: PMC3424429. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3424429/
- National Health Service (NHS) Erythema Nodosum (2020) https://www.nhs.uk/conditions/erythema-nodosum/
- Rogler G, Singh A, Kavanaugh A, Rubin DT. Extraintestinal Manifestations of Inflammatory Bowel Disease: Current Concepts, Treatment, and Implications for Disease Management. Gastroenterology. 2021 Oct;161(4):1118-1132. doi: 10.1053/j.gastro.2021.07.042. Epub 2021 Aug 3. PMID: 34358489; PMCID: PMC8564770. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8564770/
- Cheng K, Faye AS. Venous thromboembolism in inflammatory bowel disease. World J Gastroenterol. 2020 Mar 28;26(12):1231-1241. doi: 10.3748/wjg.v26.i12.1231. PMID: 32256013; PMCID: PMC7109271. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7109271/
- National Health Service (NHS) Diagnosis Ulcerative colitis (2022) https://www.nhs.uk/conditions/ulcerative-colitis/diagnosis/
- National Health Service (NHS) Complications Ulcerative colitis (2022) https://www.nhs.uk/conditions/ulcerative-colitis/complications/
- National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Primary Sclerosing Cholangitis (2022) https://www.niddk.nih.gov/health-information/liver-disease/primary-sclerosing-cholangitis
- Mintz R, Feller ER, Bahr RL, Shah SA. Ocular manifestations of inflammatory bowel disease. Inflamm Bowel Dis. 2004 Mar;10(2):135-9. doi: 10.1097/00054725-200403000-00012. PMID: 15168814. https://pubmed.ncbi.nlm.nih.gov/15168814/
- Ulcerative Colitis: Symptoms, Causes, and Diet
- What is Ulcerative Colitis?
- Causes
- Symptoms
- Impact of ulcerative colitis on other organs
- Diagnosis
- Treatment
- Diet for ulcerative colitis
- Complications
- Is it possible to completely cure ulcerative colitis?
- How are ulcerative colitis and Crohn's disease different?
- When should you see a doctor?