Clotted blood may break loose and travel with blood flow to different body parts, blocking the flow in the critical blood vessels and posing a life threat.
Symptoms of thrombosis vary depending on the location of the clots. In most severe cases, when the clots break from their original formation place and travel to the blood vessels of the heart, lung, or brain, they may include shortness of breath, breathing difficulties, chest pain, or stroke symptoms.
Some medical conditions and other risk factors increase the chances of blood clots forming in the body. It’s essential to know the risk factors and be aware if you have a reason to suspect you have this condition.
Causes
Thanks to complex mechanisms, blood remains fluid and can circulate in the body’s arteries and veins without leaking out. One such crucial mechanism is hemostasis, a set of many factors that balance the clotting and dissolution of clot systems. In this state, the blood is liquid—it can circulate in the vessels but does not overflow from them. Understanding this balance is vital to understanding thrombosis and its prevention.
A properly functioning hemostasis in the event of damage or injury allows the vessel to stop bleeding by producing a clot. It also prevents the clot from forming in the vessel lumen, limiting blood flow. In the case of hemostasis abnormalities, excessive bleeding or excessive clot formation, i.e., thrombosis, may develop.
The interaction of platelets and a set of blood proteins is necessary for proper blood clotting. Platelets stick together and form a plug in the place of the damaged vessel, initially preventing the outflow of blood. However, this plug is unstable and requires additional stabilizing factors; otherwise, the bleeding would quickly return.
Various conditions, medications, or lifestyle factors may cause thrombosis. Generally, many factors contribute to the blood clot formation inside the vessel. Experts distinguish three main factors that lead to thrombus development, also called Virchow’s triad. Those include:
- Vascular wall damage (e.g., as a result of injury or lower limb surgery)
- Slowing down of blood flow (e.g., due to limb immobilization or vein compression)
- The predominance of clotting factors over clot-dissolving factors in the blood
People exposed to the risk factors usually do not feel sick and are unaware of the threat. Often, it is only when disturbing symptoms appear that they discover the existence of a disease such as a thrombosis. Because of that, it’s essential to know the situations predisposing to the described cause mechanisms to see if you are at risk.
Taking certain medications, especially those containing estrogens, such as contraceptive pills or hormone replacement during menopause, makes your blood thicker, which may lead to thrombosis. Suppose a woman who is on contraceptive pills starts smoking tobacco, which is another crucial risk factor for blood clots. Then, having two major risk factors simultaneously, the risk is many times higher. Therefore, it’s important to discuss the risk with your doctor before starting estrogen therapy.
Types
There are two main types of thrombosis:
- Venous thrombosis occurs when a blood clot forms inside a vein. Veins carry blood from the entire body to the heart. Their walls are thin, and the blood inside them has low pressure. This type of disease is the most common long-lasting thrombosis and most commonly happens in leg veins. It is more common in older people as veins weaken, leading to blood stagnation.
- Arterial thrombosis involves a blood clot forming in the artery, a vessel carrying blood from the heart to the entire body. Blood in the arteries is rich in oxygen and nutrients, and the walls of the arteries are thick as the blood flows inside them with high pressure. Arterial thrombosis is responsible for conditions such as stroke and heart attack.
Symptoms
The symptoms of thrombosis depend on where the blood clot is located (veins, arteries, or heart chamber), how big it is, whether it limits blood flow or completely blocks the vessel, and whether it is chronic or acute. Sometimes, long-lasting thrombosis remains unnoticed for a long time, and its complications are the first symptoms you notice.
Veins (Deep Vein Thrombosis – DVT)
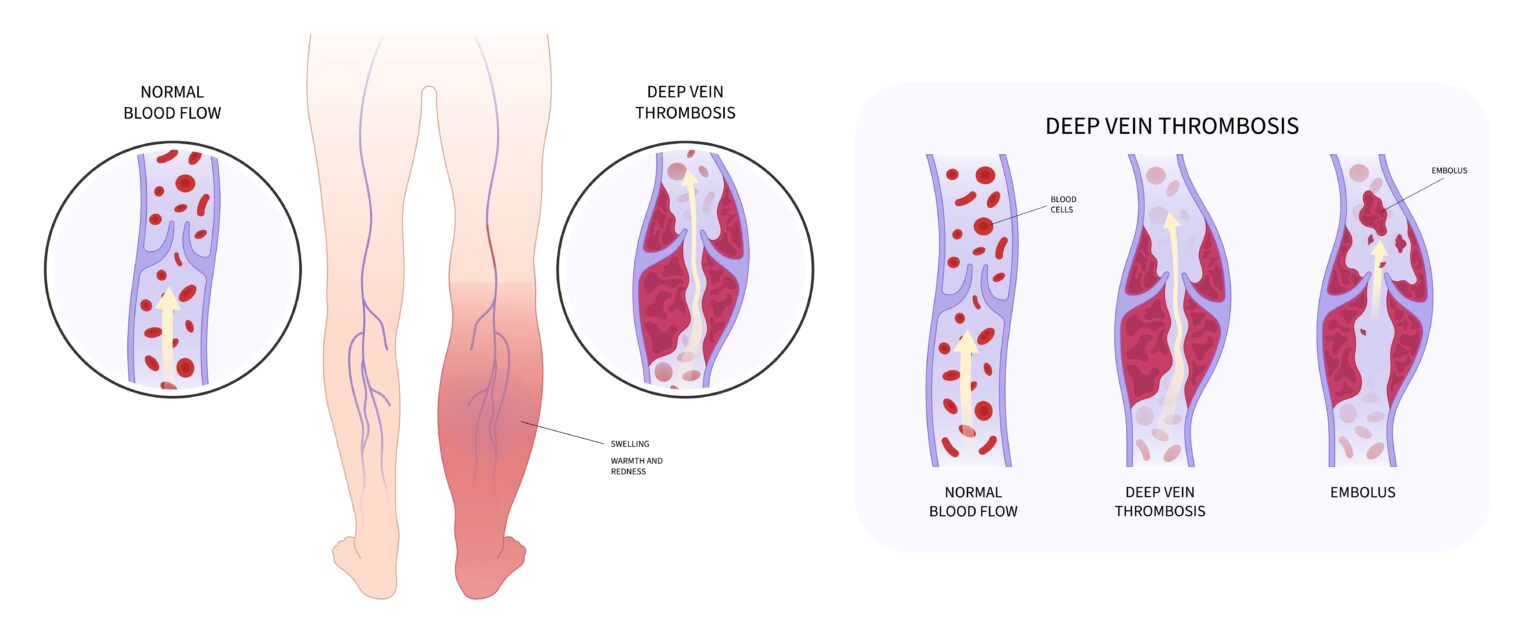
When a blood clot forms inside the deep veins of the legs, it’s called deep vein thrombosis (DVT). The deep veins of the lower limbs carry blood from the entire body to the heart. They are located between the muscles in the calf and thigh.
The deep veins play an important role because they drain most of the blood from the legs. Various conditions that block blood from flowing efficiently through the veins contribute to developing deep vein thrombosis. Symptoms of DVT include:
- Swelling, usually in one leg
- Throbbing pain in part of the limb (e.g., in the calf or under the knee), which disappears or improves when the leg is raised
- Painful, warmed-up area of the skin
- Red or darkened and tense skin (might be difficult to notice on brown skin)
- Swollen and painful veins
Blood Clot in The Artery
Thrombosis can also happen in the artery (the vessel that transports blood rich in oxygen and nutrients to the body’s cells). Artery thrombosis can occur suddenly (acute) or be long-lasting (chronic), further limiting blood supply. Thrombosis of the artery most commonly happens in the leg arteries but can also occur in the arm or belly.
Symptoms of sudden artery ischemia, which is the inadequate blood supply of the legs, include:
- Pain in the affected limb
- No pulse peripherally from the clogged area
- Pale, cold skin of the affected leg
- Inability to move or severe weakness of the affected area
- Numbness
- Tissue death (necrosis) – When the leg is deprived of blood supply for long, muscles and other tissues start to die.
Sudden blockage of the leg artery happens either from thrombosis that forms in the leg due to atherosclerosis or when a blood clot from another part of the body, such as the heart chamber, breaks loose and flows into the leg artery, where it gets stuck.
Belly Thrombosis
If a blood clot, formed usually in the heart chamber, breaks loose, it may flow with the blood flow into your belly to the mesenteric artery. The mesenteric artery is the vessel that provides your intestines with blood rich in oxygen and nutrients. When blockage occurs, it can lead to small intestine ischemia and necrosis (death). It is a severe and potentially fatal condition that has to be treated by emergency surgery.
Symptoms of belly ischemia include:
- Severe stomach pain that occurs suddenly
- Having an urgent need for a bowel movement
- Vomiting
- Fever
If the symptoms build up over time (chronic belly thrombosis), the symptoms look slightly different. In such people, belly pain is the main symptom that occurs about 30 minutes after eating and gets better within 2 hours.
Heart Attack
Coronary arteries are unique vessels that provide heart muscle with oxygen and nutrients. During atherosclerosis, plaque builds up inside them, leading to further vessel blockage if left untreated. If the plaque breaks, thrombosis blocks the heart artery completely, leading to a heart attack. The heart attack symptoms include:
- Chest pain that radiates to the jaw or left arm
- Trouble breathing
- Fainting
- Nausea
Stroke or TIA (Thrombosis in The Brain)
Your brain requires a persistent supply of blood to function correctly. During atherosclerosis, plaque (a buildup of cholesterol, fats, and other substances) can build up inside the artery that delivers blood to the brain, limiting its supply. When plaque breaks, the inside of the artery gets damaged, and blood clots start forming. When a blood clot closes the blood supply completely, brain cells deprived of oxygen start dying, which is called a stroke. Symptoms of thrombosis in brain vessels include:
- Sudden weakness of facial muscles, legs, or arms on one side of the body
- Speaking difficulties
- Confusion
- Trouble with seeing (in one or both eyes)
If a stoppage in blood flow is only temporary, transient ischemic attack (TIA) occurs, which are symptoms of stroke which, however are not permanent and pass within 24 hours.
How Common Is It?
Thrombosis is a common condition. About 900,000 people in the United States are affected by deep vein thrombosis yearly. Thrombosis is less common among younger people, and its prevalence among older adults is as high as 1 per 100.
Risk Factors
Some people are at a higher risk of getting thrombosis due to their medical conditions, medications, and lifestyle habits. The risk factors include:
- Atherosclerosis
- Cancer
- Contraceptives
- Atrial fibrillation
- Being over 40 – with age, veins and venous valves are becoming increasingly insufficient. It favors blood stagnation inside them, which may lead to blood clot formation.
- Chemotherapy
- Pregnancy
- Having a family history of thrombosis or pulmonary embolism (blood clot stuck in the lungs arteries)
- Injuries, especially broken bones
- Having varicose veins
- Long plane flight
- Infections
- Obesity
- Having a medical history of heart attack or stroke
- Blood clotting diseases
- Undergoing medical procedures and surgeries concerning veins or arteries which can cause damage to the vessel wall
- Using hormone replacement during menopause
- Smoking
Diagnosis
When doctors suspect you have thrombosis, they perform physical exams and order blood and imaging tests.
During physical examination, your doctor may look and touch the affected areas to check for signs of skin discoloration, warmed skin, or swelling. They can also take your pulse in different parts of the body.
Imaging tests that can be ordered when thrombosis is suspected include:
- Doppler ultrasound – a test that allows the assessment of blood flow
- Computed tomography (CT)
- Magnetic resonance imaging (MRI)
- Angiogram

Blood tests useful in thrombosis diagnosis include:
- D-dimer blood test – D dimers are fibrin breakdown products that appear in the body when a previously formed blood clot is dissolved. Low D-dimer levels allow the exclusion of diseases such as deep vein thrombosis or pulmonary embolism.
- Blood components test, including platelet count
- Troponin tests – helpful in confirming heart attack
Treatment
Thrombosis treatment consists of medications and surgeries. Main treatments include:
- Blood thinners – drugs that reduce blood clotting. Those medications prevent the clot from getting bigger. They can’t, however, get rid of the clot that has already been formed. If your doctor prescribes those drugs, you probably will have to take them for at least three months
- Thrombectomy – surgery during which a surgeon removes a blood clot directly.
- Thrombolytic therapy is an emergency therapy for situations when thrombosis occurs in vessels critical to body functioning—used in strokes, heart attacks, and pulmonary embolism.

Complications
Complications of thrombosis depend on the location of a blood clot. The most common type of thrombosis – deep vein thrombosis (DVT) carries the risk of two main complications: pulmonary embolism and post-thrombotic syndrome.
Pulmonary Embolism
Pulmonary embolism is a complication of deep vein thrombosis. When a blood clot from the leg vein breaks loose, it travels with blood flow and can get stuck inside the lung vessel (pulmonary artery), blocking the blood supply. This situation is called pulmonary embolism, as a broken piece of clot that blocks the lung artery is called an embolus. Symptoms that may accompany it include:
- Sudden breathing difficulties
- Sharp pain in the chest
- Coughing up blood
Post-thrombotic Syndrome
Post-thrombotic syndrome is a common complication of deep vein thrombosis. After a thrombosis, permanent changes occur in the deep vein system, which causes long-lasting vein malfunction and its symptoms.
One of the early symptoms of post-thrombotic syndrome is swelling of the limb, followed by hardening of the skin tissue. The swelling is slightly painful when pressed and typically is located on the inner surface of the calf. A skin rash and skin redness also often appear. Then, in some people, varicose veins develop.
In this condition, minor injuries may result in difficult-to-heal wounds and venous ulcers. They are usually located around the ankle on the inside of the leg.
Prevention
To lower your chances of developing thrombosis, the following prevention methods can be used separately or in combination:
- Taking drugs that reduce blood clotting (blood thinners)
- Compression therapy involves using compression stockings or elastic bandages. It is essential to put on these products correctly. The pressure should gradually decrease upwards, with the most significant pressure near the ankle.
- Start moving around (like getting up and walking) as quickly as you can after you’ve had to stay still for a long time because of an operation or being sick.
- Keep your weight in check, try not to sit too much, and get active.
When Should You See a Doctor?
If you start seeing signs that worry you, such as swelling, pain, skin discoloration, or numbness, it’s important to contact your doctor, as that may suggest thrombosis.
If you experience symptoms such as chest pain, breathing difficulties, or coughing up blood, call the local emergency number, as you might be experiencing a pulmonary embolism, a hazardous complication of vein thrombosis.
Sources
- National Library of Medicine (NIH) Damilola Ashorobi; Muhammad Atif Ameer; Roberto Fernandez. Thrombosis (2023) https://www.ncbi.nlm.nih.gov/books/NBK538430/
- National Library of Medicine (NIH) Andrew LaPelusa; Heeransh D. Dave. Physiology, Hemostasis (2023) https://www.ncbi.nlm.nih.gov/books/NBK545263/
- National Library of Medicine (NIH) Eduardo Franca; Maxim E. Shaydakov; Jason Kosove. Mesenteric Artery Thrombosis (2023) https://www.ncbi.nlm.nih.gov/books/NBK539763/
- Centers for Disease Control and Prevention (CDC) Data and Statistics on Venous Thromboembolism (2023) https://www.cdc.gov/ncbddd/dvt/data.html
- National Health Service (NHS) Pulmonary Embolism (2023) https://www.nhs.uk/conditions/pulmonary-embolism/
- Adnan G, Singh DP, Mahajan K. Coronary Artery Thrombus. 2022 Oct 3. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan–. PMID: 30521229. https://pubmed.ncbi.nlm.nih.gov/30521229/
- Obara H, Matsubara K, Kitagawa Y. Acute Limb Ischemia. Ann Vasc Dis. 2018 Dec 25;11(4):443-448. doi: 10.3400/avd.ra.18-00074. PMID: 30636997; PMCID: PMC6326052. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6326052/
- Ogata J, Masuda J, Yutani C, Yamaguchi T. Mechanisms of cerebral artery thrombosis: a histopathological analysis on eight necropsy cases. J Neurol Neurosurg Psychiatry. 1994 Jan;57(1):17-21. doi: 10.1136/jnnp.57.1.17. PMID: 8301298; PMCID: PMC485034. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC485034/
- Farrell JJ, Sutter C, Tavri S, Patel I. Incidence and interventions for post-thrombotic syndrome. Cardiovasc Diagn Ther. 2016 Dec;6(6):623-631. doi: 10.21037/cdt.2016.11.22. PMID: 28123982; PMCID: PMC5220207. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5220207/
- Centers for Disease Control and Prevention (CDC) Diagnosis and Treatment of Venous Thromboembolism (2023) https://www.cdc.gov/ncbddd/dvt/diagnosis-treatment.html
- National Health Service (NHS) DVT (deep vein thrombosis) (2023) https://www.nhs.uk/conditions/deep-vein-thrombosis-dvt/