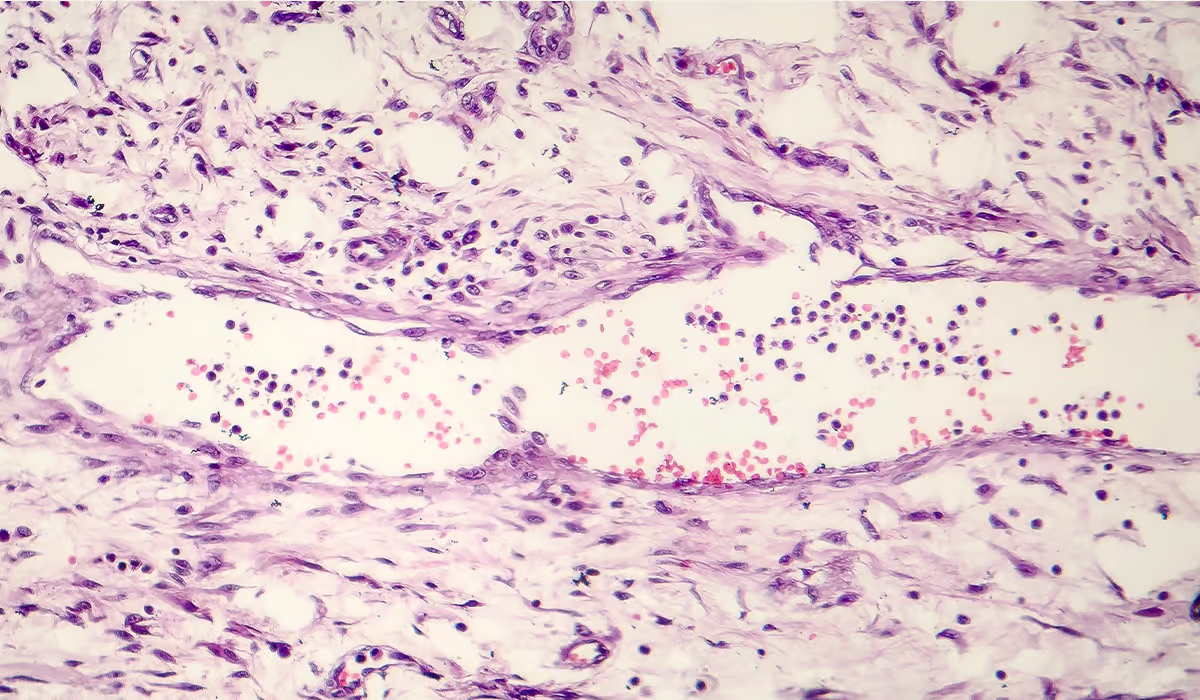
Scleroderma’s progression is unique to each individual, leading to various complications for each person affected by the disease. Although it usually affects the skin, symptoms can appear in any body part. During the disease, the body starts to produce and accumulate too much collagen, thickening tissue. Collagen is a protein essential for the body’s correct functioning. However, when it is overproduced, the tissues become thicker and more fibrous than they should.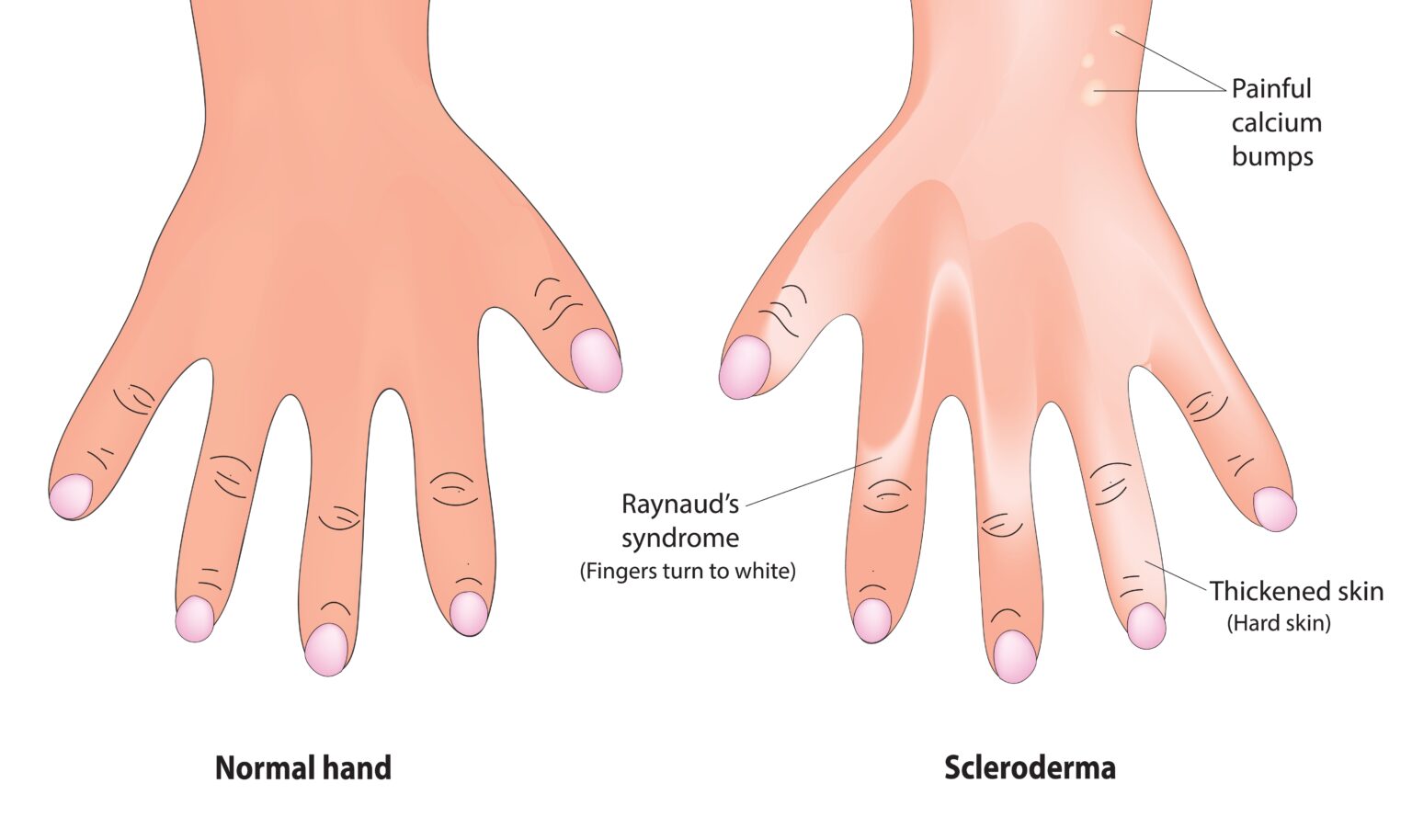
Types
There are several types of scleroderma. Physicians distinguish two main types of the condition: localized and systemic.
Localized
A localized type (sometimes called morphea) of the disease is only present in one place on the body, usually the skin. Skin lesions are typically noticed in the hands and feet and then progress slowly upwards. In most cases, lesions don’t extend beyond the knees and elbows. They are itchy and tender. With time, lesions develop a hard center with a violet border. This type can occur both in children and adults.
Additionally, symptoms such as weakness, sudden redness, and finger pain (Raynaud’s phenomenon) may occur. Most skin lesions resolve independently in a few years but can leave skin discolored.
Several subtypes of localized scleroderma have different affected areas and complications, such as joint abnormalities. In the subtype called linear morphea, skin lesions appear as thick lines around legs and arms, which may cause long-lasting problems with bones and limbs.
Systemic
In the systemic type, the disease affects organs and skin lesions. Skin lesions may appear on hands, arms, torso, and thighs. Thickening of the skin progresses quickly. Affected organs may include the lungs, kidneys (an organ that produces pee), heart, and digestive system. Usually, the more advanced the skin lesions, the more severe the organ symptoms.
The condition can be fatal. It may limit your ability to breathe or digest, leading to severe complications.
Doctors distinguish three subtypes of systemic scleroderma. Those include:
- Diffuse – Skin changes can affect skin all over the body, spreading to broad areas like the chest and abdomen. At the same time, it can affect multiple organs, including the digestive system, heart, and lungs.
- Limited (CREST)—When physicians discuss limited scleroderma, they typically refer to symptoms called the acronym CREST. Those symptoms include calcium deposits in the skin, Raynaud’s syndrome (sudden discoloration of the fingers caused by vascular problems), difficulty swallowing, thickening and tightening of the fingers, and red spots on the skin.
- Sine sclerosis is the subtype with symptoms of limited sclerosis without any skin changes.
Causes
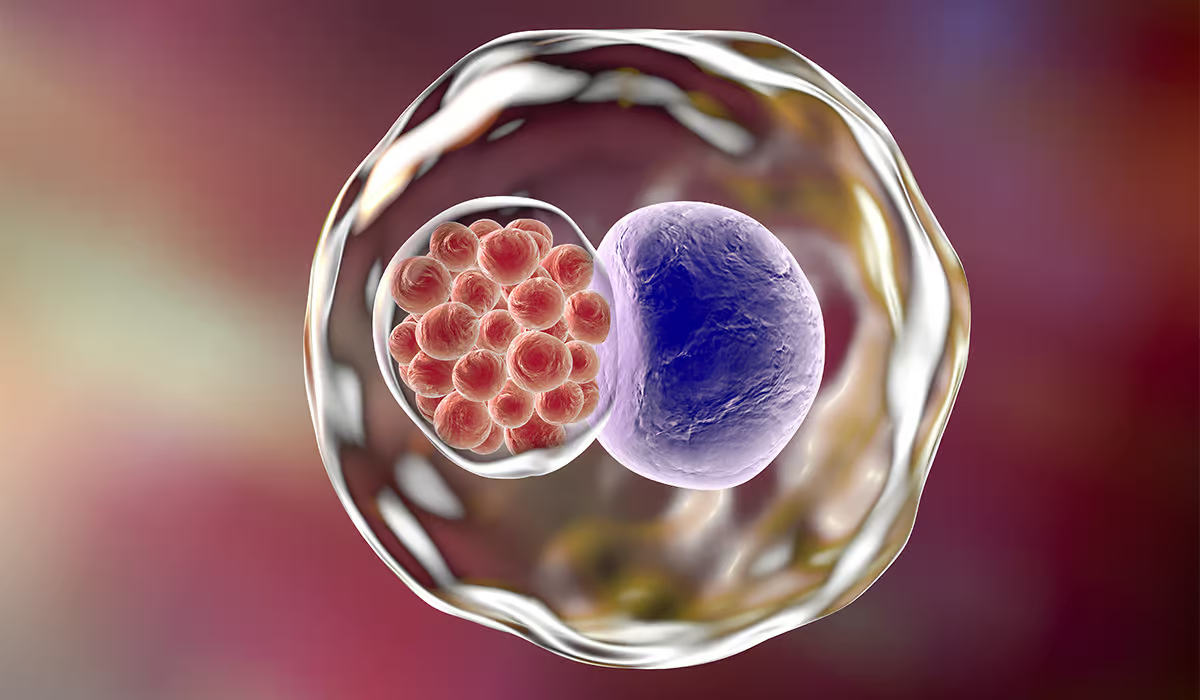
Scleroderma is an autoimmune disease, meaning the immune system produces antibodies that attack body organs. The exact cause of why the body starts producing those antibodies is not known. Experts suspect that the role in its development may play genetic and environmental factors. Environmental factors may include virus infections, exposure to chemicals, and pollution.
How Common Is It?
Scleroderma is rare. Each year, around 1 in 100,000 people develop the condition. It is more common in women than in men. The average age at which the condition develops is 30-50, but it can develop at any age.
Symptoms
The symptoms of the condition depend on the affected organs. They result from ongoing hardening of the tissues and problems with blood vessels. The main signs you’ll notice include:
- Skin becoming hard, tight, and shiny
- Stiffness in your joints, mostly when you wake up
- Joint pain
- Feeling very tired
If this condition affects different parts of your body or types of this illness, you might see some other signs, too.

Skin Changes
The biggest thing you’ll see with this illness is changes to the skin. It gets thick and stiff, doesn’t stretch like it used to, and might change color. When skin discolorations are surrounded by lighter skin, experts usually call it a “salt and pepper” appearance. Other skin changes include swelling of the fingers and skin atrophy, which is a waste away of the tissue. Additionally, calcium deposits can appear in the skin, which looks like white lumps.
Fingers and toes may become swollen, stiff, and tight, and joints of the hands and feet can become stiff and painful. Changes start at the fingertips and spread upwards.
When the face is affected, it might become tight, with loose facial expressions, and have difficulty opening the mouth or closing the eyelids. Some small blood vessels might become visible under the skin, causing discoloration.
Raynaud’s Symptom
Raynaud’s symptom is a finger blood vessel spasm. It is usually triggered by the cold or stress but can also happen independently. The symptom starts with sudden paleness and numbness in the fingers. Then, they turn bluish and painful. Finally, fingers get red with a burning sensation when a blood vessel spasm passes.
Joints and Muscles
Joint pains may appear in all types of scleroderma and are caused by inflammation. Joints can become stiff, especially in the morning. Muscles can become weak and painful because of the muscle tissue’s ongoing hardening in some types of disease.
Systemic Scleroderma
The systemic type of disease causes symptoms in the skin and organs. Skin changes typically affect more extensive areas, with Raynaud’s syndrome present. Affected organs may include:
- Digestive system – Symptoms can be heartburn, diarrhea, constipation, and bloating.
- Esophagus (the tube that passes food from the mouth to the stomach) – An Affected esophagus can become stiff and narrow, resulting in difficulty swallowing.
- Lungs – When the disease affects the lungs, shortness of breath, coughing, and poor tolerance to physical exertion may appear.
- Kidneys – Kidney failure and hypertension can develop as a result of the disease.
- Heart – Hardening of the heart walls can lead to heart failure, abnormal heartbeat, and fluid buildup around the organ.
Risk Factors
Some people are at a higher risk for sclerosis development. The risk factors include:
- Being a woman – Females are about three times more likely to develop scleroderma than men.
- Age between 45 and 64—Although the condition can develop at any age, most people get it between 45 and 64.
- Family history of scleroderma – If someone in your family has this condition, you are at higher risk of developing it.
- Exposure to chemical substances
- Exposure to heavy metals
- Being black – Black people are at the highest risk of disease development among all races. The symptoms also tend to be more severe in this group.
Although experts distinguish factors that raise the chances of sclerosis development, it is impossible to prevent the condition as the exact cause of the disease remains unknown.
Diagnosis
Dermatologists and rheumatologists typically diagnose scleroderma. Dermatologists treat conditions affecting the skin, and rheumatologists treat joint and autoimmune diseases. The disease is challenging to diagnose as it is rare, and the symptoms are similar to those in other conditions.
First, the doctor assesses your symptoms and asks about a family history of autoimmune conditions. Next, the physician performs a physical exam and may order some tests:
- Blood tests – Your physician may order tests for antibodies characteristic of the condition.
- Skin biopsy – Taking a small skin sample to evaluate under the microscope makes it possible to find changes typical of sclerosis.
- CT scans – These scans let doctors see a clear image of what’s inside your body. Lung tests – Doctors use these to check how well your lungs work.
- Echocardiogram – This is a heart ultrasound that helps doctors look at how your heart is built and how it works.
- Endoscopy – This test checks if the disease has impacted the esophagus for some scleroderma patients.
Treatment
There is no cure for scleroderma. However, medications, physical therapy, and lifestyle changes can alleviate symptoms and help prevent complications.
Medications
Managing symptoms of scleroderma involves multiple medications, as the disease may affect any body part. If you have scleroderma, the following medications may be prescribed to you by your physicians:
- Drugs that dilate blood vessels – The narrowing of the blood vessels causes Raynaud’s phenomenon.
- Painkillers
- Immunosuppressants – Drugs that suppress the immune system help slow down the disease.
Physical Therapy
Physical therapy is super important when you’re dealing with scleroderma. It includes different exercises and treatments that keep you moving and reduce stiffness. It also helps you do everyday things by yourself.
Lifestyle Changes
There are things you can do that might slow down the disease and make your symptoms easier to handle. For example:
- Stopping smoking can help a lot because smoking makes the small blood vessels tighter, which makes Raynaud’s symptoms a lot worse.
- Sun and cold protection—Since scleroderma affects the skin, it’s essential to protect it as well as possible. Protection from the cold is necessary, as the cold triggers Raynaud’s symptom.
- Use sunscreen – Avoiding sun baths and using sunscreen is essential in managing scleroderma. It protects the skin from further irritation and dryness.
- Exercise gently – Staying active can relieve joint and muscle stiffness, common symptoms of the condition.
- Moisturize your skin – Hardening skin is the most characteristic symptom of the condition. To alleviate it, you can use moisturizer.
Complications
People with scleroderma are much more likely to develop Sjögren’s syndrome, another autoimmune condition where salivary and tear glands aren’t working as they should, leading to dry mouth and eyes. Other complications that might occur include:
- Pulmonary hypertension – High blood pressure in the vessels supplying the lungs with blood
- Kidney failure
- Heart complications, including irregular heartbeat, heart failure, and heart attack
- Gastrointestinal conditions, such as poor absorption of food or permanent narrowing of the esophagus
- Weak immune system
- Cancer
- Permanent joint stiffness
Sometimes, complications of the condition may be life-threatening. If you experience any symptoms that may suggest that conditions such as kidney failure or a heart attack are developing, call for emergency medical attention. Symptoms that should especially worry you include chest pain, very high blood pressure, shortness of breath, difficulty swallowing, or sudden loss of consciousness.
Prognosis
Scleroderma is a chronic autoimmune condition. It cannot be completely cured, and the exact cause is unknown. Once the disease damages the tissue, it’s irreversible.
The treatment aims at alleviating symptoms and preventing complications.
When Should You See a Doctor?
If you notice symptoms of scleroderma, such as Raynaud’s symptoms or hardening of the skin on your hands and feet, you should contact your doctor. The most characteristic symptoms of the disease are skin changes. Symptoms such as muscle or joint pain can be present in several conditions, but it is a good idea to mention it to your physician if you’re experiencing it.
If you have been diagnosed with scleroderma and experience symptoms such as very high blood pressure, vision problems, chest pain, or consciousness disorders, contact emergency medical help as it may suggest you developed life-threatening complications of your condition.
Sources
- National Health Service (NHS) Scleroderma (2023)
https://www.nhs.uk/conditions/scleroderma/ - Kowalska-Kępczyńska A. Systemic Scleroderma-Definition, Clinical Picture and Laboratory Diagnostics. J Clin Med. 2022 Apr 20;11(9):2299. doi: 10.3390/jcm11092299. PMID: 35566425; PMCID: PMC9100749.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9100749/ - Singh A, Ambujam S, Varghese A, Vishranth SP, Sadanandan N. Salt-and-pepper Appearance: A Cutaneous Clue for the Diagnosis of Systemic Sclerosis. Indian J Dermatol. 2012 Sep;57(5):412-3. doi: 10.4103/0019-5154.100512. PMID: 23112372; PMCID: PMC3482815.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3482815/ - National Library of Medicine (NIH) Gopi K. Penmetsa; Amit Sapra. Morphea (2023)
https://www.ncbi.nlm.nih.gov/books/NBK559010/ - Careta MF, Romiti R. Localized scleroderma: clinical spectrum and therapeutic update. An Bras Dermatol. 2015 Jan-Feb;90(1):62-73. doi: 10.1590/abd1806-4841.20152890. PMID: 25672301; PMCID: PMC4323700.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4323700/ - Abbot S, Bossingham D, Proudman S, de Costa C, Ho-Huynh A. Risk factors for the development of systemic sclerosis: a systematic review of the literature. Rheumatol Adv Pract. 2018 Oct 11;2(2):rky041. doi: 10.1093/rap/rky041. PMID: 31431978; PMCID: PMC6649937.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6649937/ - Sobolewski P, Maślińska M, Wieczorek M, Łagun Z, Malewska A, Roszkiewicz M, Nitskovich R, Szymańska E, Walecka I. Systemic sclerosis – multidisciplinary disease: clinical features and treatment. Reumatologia. 2019;57(4):221-233. doi: 10.5114/reum.2019.87619. Epub 2019 Aug 31. PMID: 31548749; PMCID: PMC6753596.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6753596/ - Pope JE. Scleroderma overlap syndromes. Curr Opin Rheumatol. 2002 Nov;14(6):704-10. doi: 10.1097/00002281-200211000-00013. PMID: 12410095.
https://pubmed.ncbi.nlm.nih.gov/12410095/ - Van Praet JT, Smith V, Haspeslagh M, Degryse N, Elewaut D, De Keyser F. Histopathological cutaneous alterations in systemic sclerosis: a clinicopathological study. Arthritis Res Ther. 2011 Feb 28;13(1):R35. doi: 10.1186/ar3267. PMID: 21356083; PMCID: PMC3241379.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3241379/ - National Institute of Arthritis and Musculoskeletal and Skin Diseases (NIAMS) Scleroderma: Diagnosis, Treatment, and Steps to Take (2023)
https://www.niams.nih.gov/health-topics/scleroderma/diagnosis-treatment-and-steps-to-take