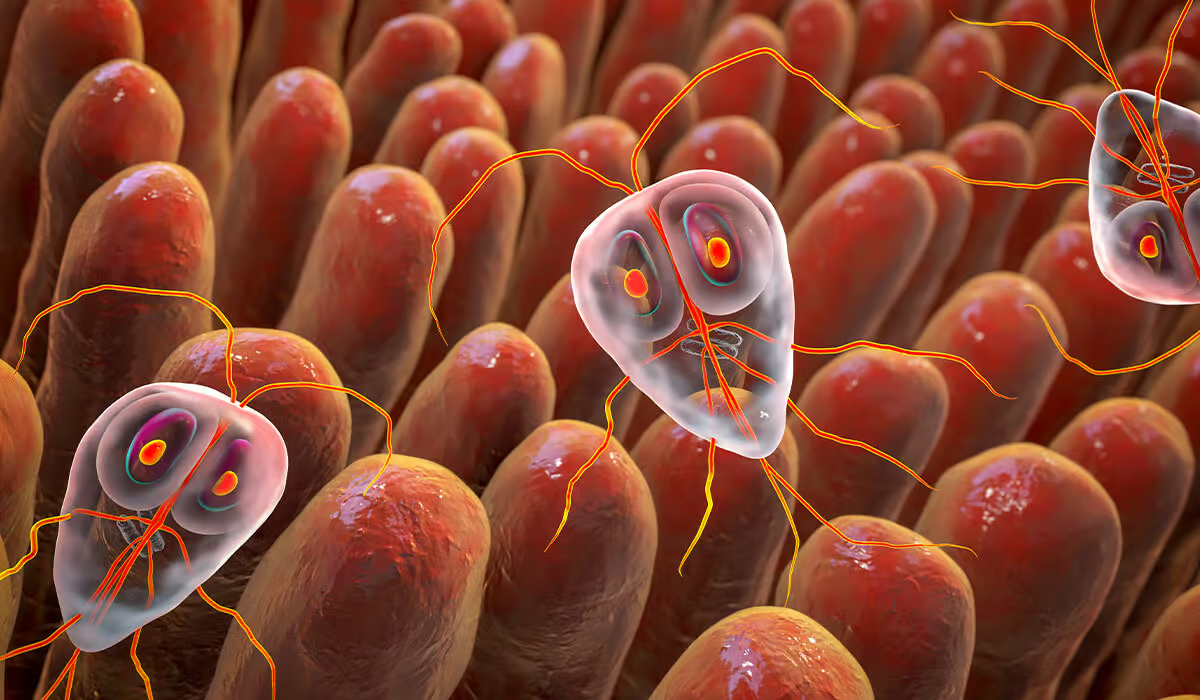
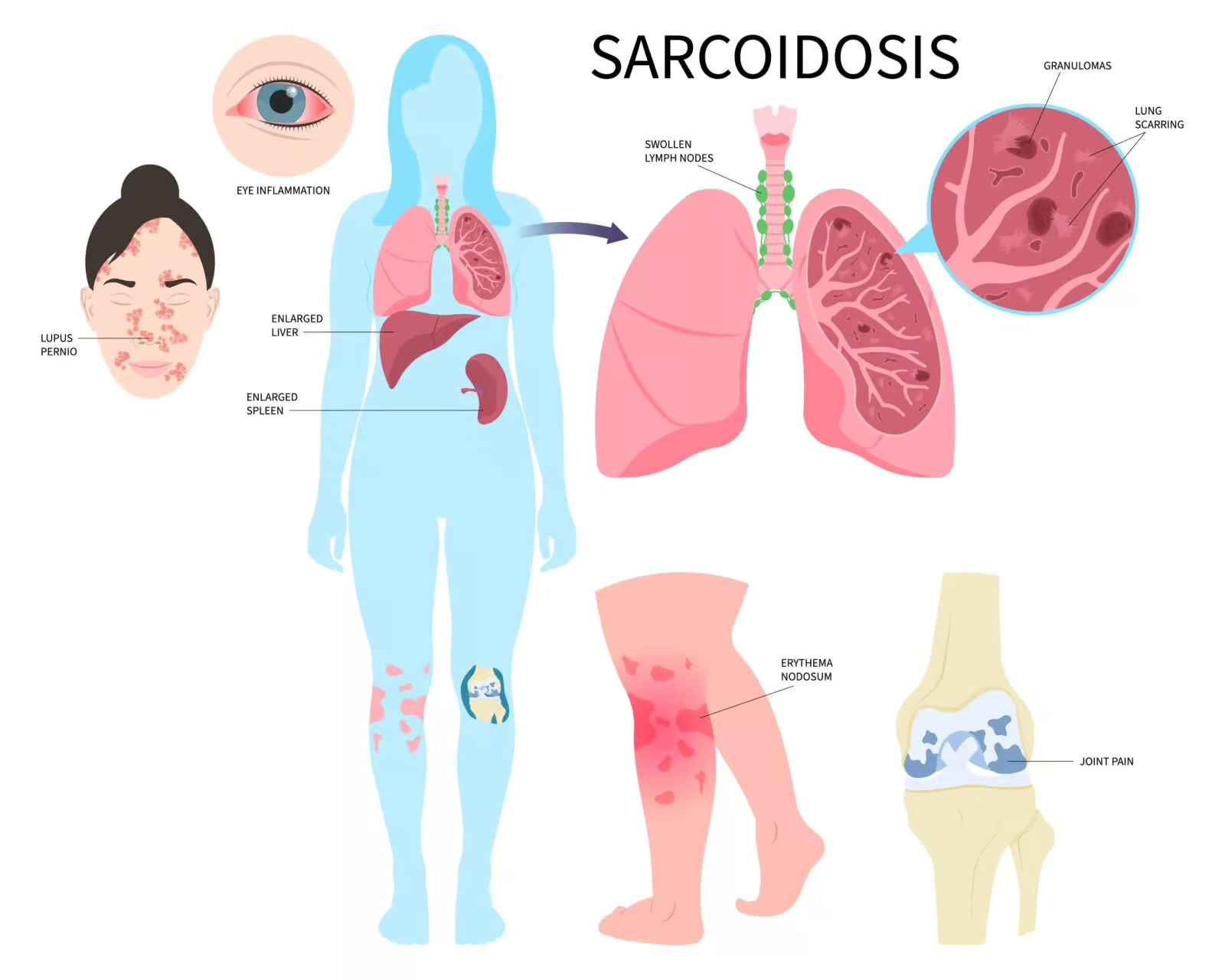
They arise from white blood cells (primarily lymphocytes and macrophages), which, unlike tuberculosis, do not undergo caseation. Because the disease most often affects the lungs and mediastinal lymph nodes, impairing gas exchange, it is also classified as interstitial lung disease. Sarcoidosis can also attack other organs, such as the heart, liver, muscles, joints, spleen, eyes, etc., causing dysfunction.
Causes
The causes of sarcoidosis are unknown. Scientists suspect that the immune system’s reaction to an unidentified antigen (a substance in the body detected by specific immune system cells) is responsible for developing the disease. The antigen can also stimulate the production of antibodies directed against itself.
Sarcoidosis can be influenced by genetic factors and the presence of the disease in one’s family. In fact, relatives of individuals with sarcoidosis have a four times higher risk of developing the disease.
In addition to genetic predisposition, infection also plays a role in sarcoidosis. There is suspicion that certain bacteria, such as those causing tuberculosis, as well as various viruses, may contribute to the development of sarcoidosis. Moreover, prolonged exposure to organic dust, mold, pesticides, or working in industries involving metal and stone processing are other potential triggers of sarcoidosis.
How Common Is It?
Sarcoidosis is a rare condition that affects around 150,000 to 200,000 individuals in the United States. Among different racial groups, black women have the highest incidence rate of this disease.
Symptoms
Sarcoidosis may be asymptomatic. Approximately 50-70% of patients experience general symptoms, the so-called non-specific symptoms, which include:
- Fever
- Fatigue
- Weakness
- Loss of appetite
- Weight loss
- Malaise
- Night sweats
Symptoms may concern the organ in which the disease develops and may only occur periodically. Up to 90% of cases involve sarcoidosis of the lungs and lymph nodes, and therefore the symptoms usually include:
- Cough
- Shortness of breath
- Wheezing
- Various forms of chest pain, e.g., pressure, burning
- Enlarged lymph nodes can be observed as palpable lumps and masses in the neck, armpits, and sometimes in the groin.
The onset of the disease may be acute, with fever, joint pain, and skin lesions. The accompanying skin lesions are called erythema nodosum. Erythema nodosum is a reddish-violet patch of various sizes on the skin, sometimes warmer than healthy skin, which disappears without leaving scars but with discoloration that lasts for weeks. They are often located on the lower legs, sometimes thighs, buttocks, and other body parts.
Much less frequently, sarcoidosis affects the nervous system, heart, eyes, and salivary glands. The symptoms are then related to damage to the affected organ.
Which Organs Are Affected by Sarcoidosis?
Lungs
This condition can affect most organs in the body. Most often (in 90% of patients), it attacks the lungs and lymph nodes in the lung cavities. This manifests as shortness of breath, cough, and chest pain when moving or resting.

Skin
Skin sarcoidosis is a relatively common manifestation of this disease. Its characteristic feature is the appearance of erythema nodosum – a significant, painful red inflammatory rash, most often on the front surface of the lower legs. Others include papular lesions, small underskin nodules, ulcers, discoloration, and alopecia.
Heart
The disease also attacks the heart and may lead to the appearance of fluid around the heart, heart rhythm abnormalities and function disturbances.
Eyes
The eyes are another organ that may be affected by the disease. The middle layer of the eye becomes inflamed, causing redness and pain. Eye symptoms may include:
- Eye burning
- Itch
- Pain
- Dry eyes
- Red eyes
- Vision problems such as seeing black spots or blurred vision
- Sensitivity to light
- Small yellow bumps on the eye
Salivary Glands
The disease also affects the salivary glands, i.e., large glands that produce saliva, causing them to swell and become painful.
Others – Joints, Nerves
Sarcoidosis can sometimes result in inflammation of the nerves, which can lead to impaired function. This can cause pain, reduced sensation, and weakened muscle strength. Individuals with this condition may also experience joint pain in the knees, ankles, and elbows. Enlargement and pain in the spleen and liver and swelling of the lymph nodes at the back of the head are other possible effects of sarcoidosis.
In certain cases, the onset of sarcoidosis can be acute, with symptoms such as fever, joint pain, skin lesions, and an enlargement of the lymph nodes near the lungs. This cluster of symptoms is known as Lofgren’s syndrome.
Risk Factors
The exact cause of sarcoidosis is still unknown. However, the development of the disease appears to be related to genetic and environmental factors. A person genetically predisposed to the disease may manifest it if they encounter triggering environmental factors.
The following risk factors may contribute to the induction of the disease:
- Working or living in a moldy or dusty environment
- Working with insecticides
- Being a woman
- Age between 30 and 50
- The condition is more common among black Americans and Scandinavian descent.
- Genetic factors – if someone in your family suffers from sarcoidosis
- Other medical factors – Having lymphoma increases your chances of getting the disease
- Medications – medications used to treat people with HIV or cancer
- Exposure to smoke from burn pits in people working in the military
Diagnosis
Sarcoidosis comes in two forms:
- Acute – which develops mainly in young people and, in most cases, resolves spontaneously,
- Chronic – primarily affecting older people.
Since the disease can attack any organ, certain functional deviations may be observed in various laboratory tests.
Blood tests that show abnormalities in the disease include, for example:
- Total blood count (may reveal anemia, i.e., too little red blood cells or hemoglobin)
- Potassium level
- High level of antibodies
- Test to check kidney function
- Hormone levels
Diagnosis of the disease is based mainly on imaging tests and biopsies of affected tissues, which can ultimately confirm the diagnosis. The most common samples are taken from the lymph nodes, lungs, conjunctiva (the membrane on the eye’s front surface), liver, kidneys, and skin.
In addition to blood tests, the following help diagnose the disease:
- Chest X-ray – Using chest X-ray, it is possible to determine the degree of advancement of pulmonary lesions according to a four-grade scale, where grade 1 is enlargement of the chest lymph nodes without lung changes, and grade 4 is advanced lung lesions, including scarring.
- Computed tomography (CT) of the chest, which may reveal the spread of nodules in the lungs and enlargement of the chest lymph nodes
- Magnetic resonance imaging, which allows to assess the involvement of other organs, mainly the central nervous system and the heart,
- Abdominal ultrasound to assess the liver, spleen, and urinary system,
- ECG – heart function test, helpful in determining possible arrhythmias,
- Ophthalmological examination to look for changes in the eye
- Analysis of cerebrospinal fluid, which helps detect abnormalities in the number of white blood cells and increases in protein levels if the central nervous system is affected,
- TB skin test to exclude tuberculosis infection
Treatment
Not everyone with sarcoidosis requires treatment. For some individuals, the condition resolves itself without intervention. However, when treatment is necessary, the objective is to attain remission, whereby the disease remains present in the body but does not provoke any symptoms. The specific treatment methods depend on the symptoms displayed and the organs affected.
Medicine
The primary treatment for sarcoidosis, a condition characterized by abnormal immune responses, is corticosteroid medication. This type of medicine helps to suppress the immune system reactions. There are various types of steroid medicine: pills, topical medication, eye drops, injections, or drugs administered by inhalation.
Like every medication, corticosteroids, when used long-term, have side effects. These include:
- High blood pressure
- High blood sugar
- Cataract (cloudy eye)
- Glaucoma (high pressure inside the eye)
- Weight gain
- Mood swings
- Osteoporosis
- Oral thrush and hoarse voice (when administered by inhalation)
Other drugs used to lower the immune system activity during the disease include:
- Immunotherapy – uses antibodies that attack the immune system’s parts and lower its activity. These drugs are administered through IV, and their most common side effects are heart problems, low blood count, or a higher chance of getting some types of cancer.
- Malaria medications
- Rheumatoid arthritis medications taken as a pill or shot

Can Sarcoidosis Be Cured?
The disease has a good prognosis. In the most common form of the disease, it usually regresses without treatment. Clinical studies have shown that the condition disappears spontaneously within two years in most patients. In other cases, it may progress and gradually impair the functioning of the respiratory system. In about 5% of cases, it ends in death. This usually occurs due to impaired lung function, central nervous system involvement, or heart failure.
Complications
Since sarcoidosis can affect various organs, its complications may concern any of them.
Lungs Complications
If the disease remains untreated for an extended period, it can lead to permanent scarring of the lungs (pulmonary fibrosis) and pulmonary hypertension. Those conditions cause breathing difficulties.
Eyes Complications
If the disease affects the eyes, it can lead to blindness since the retina may become damaged. Sarcoidosis, at times, can lead to the development of glaucoma, a condition characterized by increased pressure within the eye, or cataracts, which cause cloudiness in the eyes.
Kidney Complications
Excessive calcium in the body can disrupt calcium metabolism and cause various health issues, including the formation of kidney stones and impaired kidney function. In severe cases, this can even result in kidney failure.
Heart Complications
Sarcoidosis affects the heart by forming granulomas, leading to irregular heart rhythms and hindering blood flow. This can ultimately impair the heart’s ability to function correctly, and in some rare cases, it can even be fatal.
Nervous System Complications
Some individuals with sarcoidosis may experience complications involving their central nervous system when granulomas develop in the brain and spinal cord. One potential effect is inflammation in the facial nerves, which can lead to facial paralysis.
Prevention
The cause of sarcoidosis remains a mystery, making prevention impossible. However, certain measures can assist in preventing symptoms in individuals who are more susceptible to the disease. These include:
- Avoiding environments with mold and dust
- Staying away from insecticides
- Maintaining a healthy diet and active lifestyle to reduce the risk of infections
Is Sarcoidosis Cancer?
Sarcoidosis, due to its often non-specific symptoms, may raise the suspicion of cancer. Both lung cancer and sarcoidosis contribute to night sweats. The same applies to other symptoms such as weight loss, fatigue, cough, or chest pain. Also, changes similar to both diseases may be visible in imaging tests, such as lung X-rays. All this can worry the patient, who often begins to ask the question, is sarcoidosis a cancer?
However, these are two significantly different diseases. Sarcoidosis results from immune system disorders of unknown origin and is a lung disease. Lung cancer, however, has a genetic basis and uncontrolled division of cancer cells.
Living With Sarcoidosis
Ongoing Care
Living with sarcoidosis can be quite a challenge. If you have this condition, it’s important to regularly visit your doctor for ongoing care, even if you’re not currently experiencing any symptoms. Keeping an eye on your body’s condition and actively monitoring for any potential side effects from long-term treatment is necessary when dealing with a chronic disease.
During remission, your healthcare provider might decide to halt the treatment. However, it’s crucial to remember that the disease can flare up again. That’s why it’s important to stay vigilant and carefully observe your body for any signs of symptoms returning. If necessary, treatment can be restarted to address any reappearance of symptoms.
Lifestyle Changes
A healthy lifestyle is beneficial because it can prevent disease progression and improve your overall well-being. Making healthy lifestyle changes involves:
- Engaging in regular physical activity
- Giving up smoking
- Maintaining a balanced diet
- Getting enough good quality sleep
Mental Health
Getting a sarcoidosis diagnosis can be stressful and make you feel depressed and worrying. If you feel overwhelmed, you must seek support from your friends and family and visit a counselor. Joining a patient support group may help you adjust to living with the disease.
When Should You See a Doctor?
If you’re experiencing symptoms of sarcoidosis, like coughing, difficulty breathing, chest pain, weight loss, fevers, or night sweats, it’s important to consult your doctor for proper diagnosis and guidance. Your doctor will closely monitor your condition to determine if it’s progressing and adjust your treatment based on your needs.
In some cases, sarcoidosis may resolve on its own without the need for treatment. However, many patients require ongoing treatment to manage their symptoms effectively.
It’s common for sarcoidosis to be treated by a team of healthcare professionals working together to provide the best possible care. Because the disease can affect many organs, you may be treated by healthcare professionals specialized in treating the lungs, heart, brain, kidneys, liver, eyes, and skin diseases.
Sources
- National Heart, Lung, and Blood Institute (NHLBI) Sarcoidosis Causes and Risk Factors (2022) https://www.nhlbi.nih.gov/health/sarcoidosis/causes
- National Health Service (NHS) Sarcoidosis (2022) https://www.nhs.uk/conditions/sarcoidosis
- Aryal S, Nathan SD. Contemporary optimized practice in the management of pulmonary sarcoidosis. Ther Adv Respir Dis. 2019 Jan-Dec;13:1753466619868935. doi: 10.1177/1753466619868935. PMID: 31409257; PMCID: PMC6696842. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6696842/
- Sève P, Pacheco Y, Durupt F, Jamilloux Y, Gerfaud-Valentin M, Isaac S, Boussel L, Calender A, Androdias G, Valeyre D, El Jammal T. Sarcoidosis: A Clinical Overview from Symptoms to Diagnosis. Cells. 2021 Mar 31;10(4):766. doi: 10.3390/cells10040766. PMID: 33807303; PMCID: PMC8066110. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8066110/
- National Library of Medicine (NIH) Falon Brown; Pranav Modi; Laura S. Tanner. Lofgren Syndrome https://www.ncbi.nlm.nih.gov/books/NBK482315/
- Rossides M, Grunewald J, Eklund A, Kullberg S, Di Giuseppe D, Askling J, Arkema EV. Familial aggregation and heritability of sarcoidosis: a Swedish nested case-control study. Eur Respir J. 2018 Aug 16;52(2):1800385. doi: 10.1183/13993003.00385-2018. PMID: 29946010. https://pubmed.ncbi.nlm.nih.gov/29946010/
- Pedroso A, Ferreira I, Chikura T. Tuberculosis and Sarcoidosis Overlap: A Clinical Challenge From Diagnosis to Treatment. Cureus. 2020 Nov 23;12(11):e11662. doi: 10.7759/cureus.11662. PMID: 33391901; PMCID: PMC7769494. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7769494/
- Arkema EV, Cozier YC. Sarcoidosis epidemiology: recent estimates of incidence, prevalence and risk factors. Curr Opin Pulm Med. 2020 Sep;26(5):527-534. doi: 10.1097/MCP.0000000000000715. PMID: 32701677; PMCID: PMC7755458. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7755458/
- American Academy of Opthalmology (AAO) Edmund Tsui, MD, Nita Bhat, MBBS, MS, Michael T Yen, MD, Nahyoung Grace Lee, MD Ocular Manifestations of Sarcoidosis (2023) https://eyewiki.aao.org/Ocular_Manifestations_of_Sarcoidosis
- Farah N, Bonham CA. Sarcoidosis in U.S. Military Veterans: Can Lessons from Those Who Have Served Shape the Future of Sarcoidosis? Ann Am Thorac Soc. 2023 Jun;20(6):788-789. doi: 10.1513/AnnalsATS.202303-201ED. PMID: 37261791; PMCID: PMC10257032. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10257032/
- Gerke AK. Morbidity and mortality in sarcoidosis. Curr Opin Pulm Med. 2014 Sep;20(5):472-8. doi: 10.1097/MCP.0000000000000080. PMID: 25029298; PMCID: PMC4326053. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4326053/
- Sarcoidosis: What Is, Causes, Symptoms, and Treatment
- What Is Sarcoidosis?
- Causes
- How Common Is It?
- Symptoms
- Which Organs Are Affected by Sarcoidosis?
- Risk Factors
- Diagnosis
- Treatment
- Can Sarcoidosis Be Cured?
- Complications
- Prevention
- Is Sarcoidosis Cancer?
- Living With Sarcoidosis
- When Should You See a Doctor?