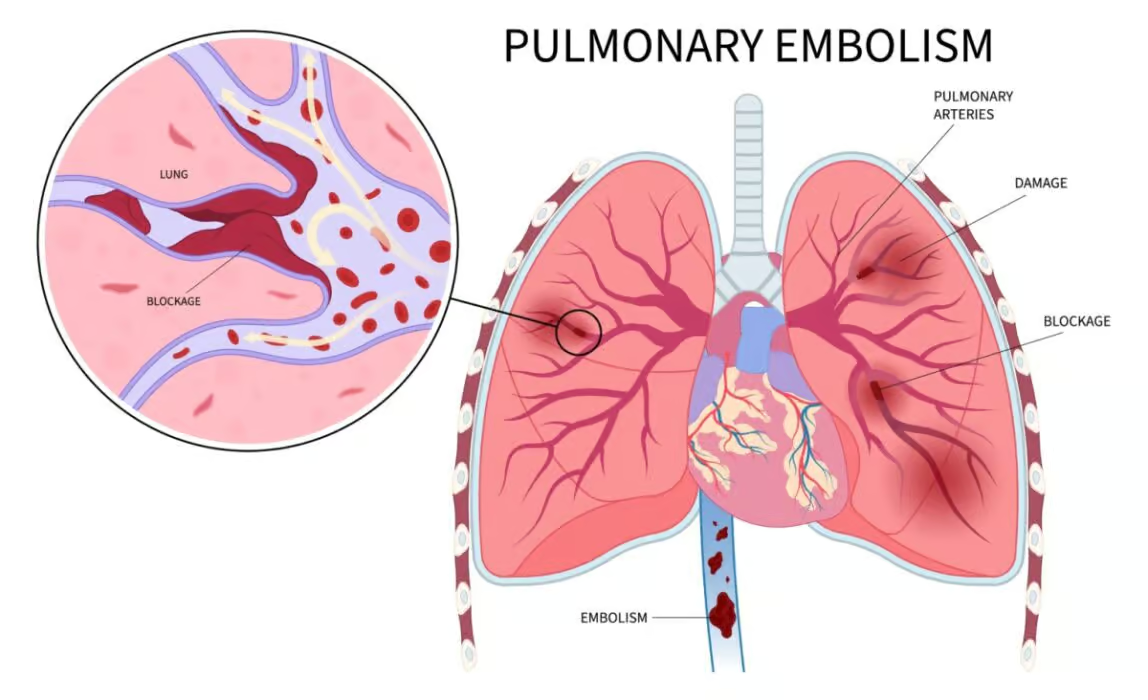
The disease usually occurs when blood clots form inside leg veins. When clots form in the deep veins of the legs, it is called deep vein thrombosis (DVT), the most significant risk factor for pulmonary embolism.
The condition blocks blood from flowing through the lungs, where it should get oxygen. That’s why it can be life-threatening. Symptoms depend on how significant the blockage is and can vary from mild symptoms to chest pain and coughing up blood.
The disease is an emergency and should be quickly treated. If left untreated, it poses a great risk of death.
How Common Is It?
Every year, 60 in 100,000 people are affected by pulmonary embolism. In the United States, it causes around 30,000 deaths yearly. Therefore, it is one of the most common blood vessel diseases.
Causes
A blockage in the lung artery causes a pulmonary embolism. It typically happens when a blood clot from the leg veins breaks free and travels through the body in the bloodstream.
Most blood clots that get stuck in the lung arteries originate from the deep veins of the legs. However, in some cases, they arise from the arm or pelvis veins. The disease in which blood clots form inside the deep veins of the legs is called deep vein thrombosis (DVT). It shouldn’t be confused with varicose veins, which is a disease involving veins on the surface. In that case, even when the blood clot develops in the superficial veins of the leg, it usually doesn’t lead to the blockage in the lungs.
Rarely, pulmonary embolism can be caused due to factors other than blood clots. Those include:
- Fat – Sometimes, a piece of fat can enter the bloodstream, leading to lung artery blockage. It may occur during some bone fractures, trauma, severe burns, or surgery.
- Infectious material
- Tumors – Rapidly growing cancer may release its fragments into the bloodstream, which travels to the lung vessels and gets stuck.
- Air – Air bubbles can get into the bloodstream during surgery, some medical procedures, or trauma
- Amniotic fluid is a fluid that surrounds and protects the fetus inside the uterus. It can get into the bloodstream during childbirth, C-section, or abortion.
Symptoms
Typically, symptoms of a lung blockage come on quickly. The most common ones include:
- Sudden shortness of breath
- Sharp chest pain
- Dry cough
- Coughing up blood
- Fainting and weakness
- Anxiety
- Sweating
- Palpitations (rapid heartbeat)
- Low blood pressure
If you start feeling these signs, your life may be in danger. Get help from emergency services right away.
Some patients simultaneously experience symptoms related to deep vein thrombosis, which may include skin redness, swelling, pain, and leg warmth.
Depending on the extent of the condition, the symptoms may strongly suggest pulmonary embolism or resemble other conditions, such as pneumonia or heart attack.
The condition can be completely asymptomatic when it affects only small lung vessels. The severity of the symptoms also depends on the condition of the heart and vessels. People who have underlying heart conditions such as heart failure tend to experience pulmonary embolism more severely than healthy people.
In this disease, due to the closure of vessels with clots and, consequently, a reduction in the amount of blood flowing through the lungs, blood oxygenation is reduced, which leads to an insufficient supply of oxygen to all organs.

Risk Factors
Some people are at a higher risk of getting pulmonary embolism than others. The most important risk factors include:
- Deep vein thrombosis
- Long periods of inactivity
- Cancer
- Hormonal birth control
Deep Vein Thrombosis
Deep vein thrombosis increases your risk of lung artery blockage, most significantly from all risk factors. During DVT, the blood clot is formed inside the deep vein of the leg. It happens due to conditions that lead to the occurrence of the so-called Virchow’s triad:
- Slowing down of blood flow
- The presence of factors that increase blood clotting
- Damage to the vascular wall (e.g., as a result of trauma or surgery on the leg)
If left untreated, a blood clot formed in the leg vein can break loose and flow with the bloodstream to the lung artery, where it gets stuck.
If you have thrombosis or experience symptoms that may suggest it (such as redness, swelling, and warmth of the leg), talk to your physician about ways you can prevent pulmonary embolism from happening.
Medical Conditions
Some other medical conditions may raise your chances of getting the disease. Those include:
- Cancer— When cancers grow in the body, they strengthen blood clotting. This happens a lot with types of cancer, like those in the pancreas, colon, stomach, brain, uterus, ovaries, and kidneys. Also, cancer treatments, like chemotherapy and radiotherapy, can increase blood clotting even more.
- Pregnancy – In the later stages, the baby can pressure veins, which makes it tough for blood to move. This can cause blood to clot.
- COVID-19 – During COVID-19 infection, the risk of lung artery blockage is higher
- Blood clotting disorders – Some genetic disorders cause excessive blood clotting.
- Surgery – Some surgeries can lead to blood clots so that you may be given anticoagulant medication after some major surgeries.
Extended Periods of Inactivity
Blood inside leg veins flows thanks to the working muscles. They work as a pump pushing the blood upwards. During long periods of inactivity, muscles aren’t working. Therefore, blood tends to stagnate in veins and doesn’t flow efficiently. Long periods of inactivity include bed rest, limb immobilization after a fracture, and long trips. Bed rest occurs after major surgeries, trauma, or during severe illnesses such as heart attack, stroke, or cancer.
Long flights typically force you to sit uncomfortably for many hours. Then, blood flow in leg veins slows down, and blood clots may appear, posing a threat of pulmonary embolism.
Other Risk Factors
- Birth control – Taking birth control pills that contain estrogen or using hormone replacement therapy can make it more likely for blood clots to form in your veins. It’s particularly important to consider this if you’re already at risk for blood clots and lung blockages.
- Smoking – Smoking cigarettes also increases the chance of getting blood clots. This is even more true if you smoke and have other things that make clots more likely.
- Being overweight—If you have excessive weight, you may also be more at risk for blood clots. Being significantly overweight can cause ongoing inflammation inside your body, which makes blood clots more likely.
Diagnosis
Doctors have various ways to determine if someone has pulmonary embolism. They start by looking at your symptoms and any risk factors you might have. Then, they do a physical check-up and ask for more tests.
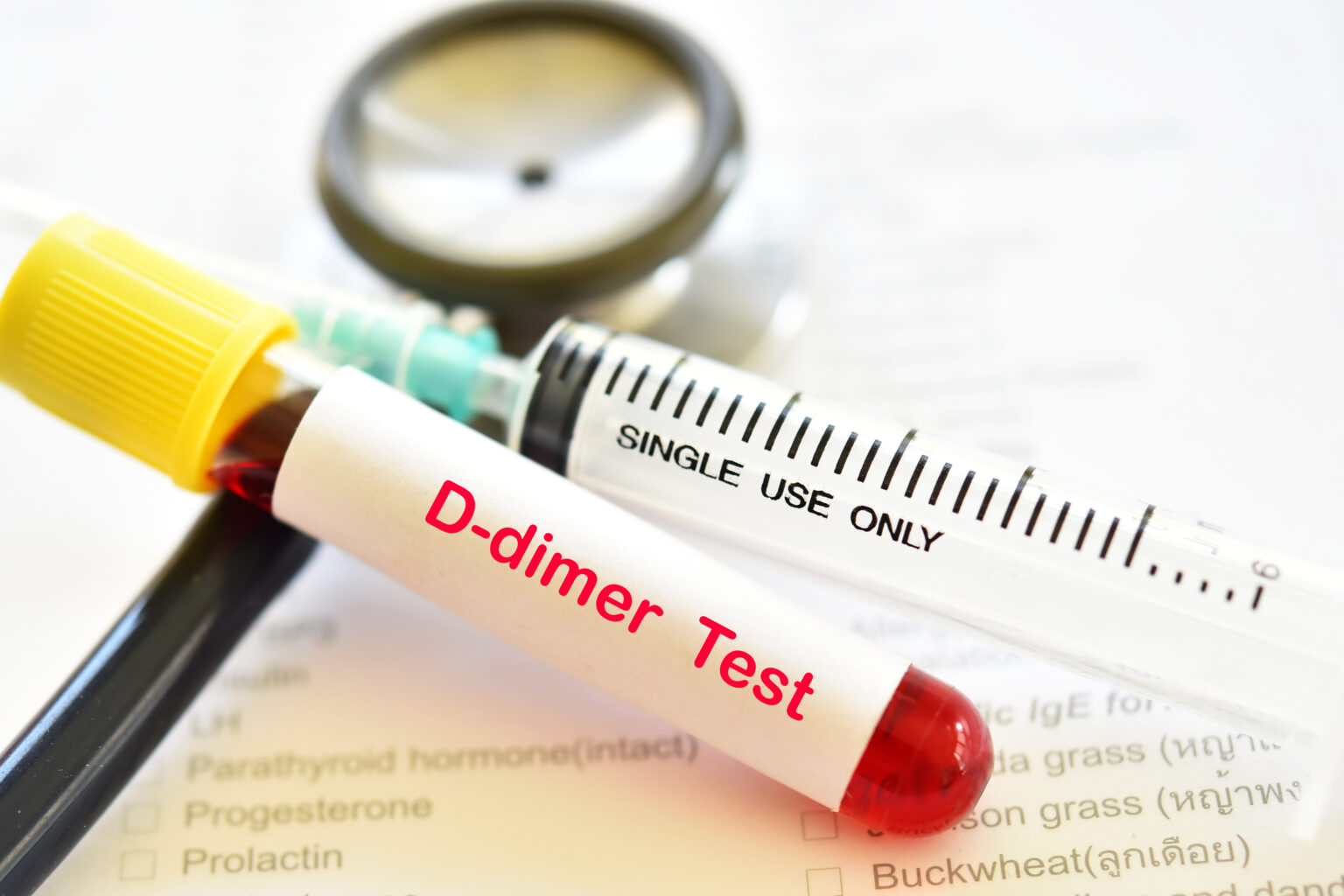
- Blood tests – A common test is the blood test called D-dimer. This is something that shows up in your blood after a clot forms. If the D-dimer level is low, it probably means that a clot isn’t causing your symptoms. But if it’s high, it doesn’t prove you have a clot because high levels can happen for other reasons, like having cancer or being pregnant.
- ECG helps differentiate a pulmonary embolism from a heart attack.
- CT (Computed tomography) angiogram – During this test, X-rays produce an image of the chest, making it possible for doctors to find conditions such as PE. The test may involve receiving contrast through the vein.
- Leg ultrasound—The most significant risk factor of PE is leg vein thrombosis, which physicians can see through a blood clot in the leg veins.
- Chest X-ray -This test uses rays to allow the physician to see a picture of the chest. It typically cannot confirm the diagnosis of PE, but it might help exclude other conditions with similar symptoms.
- MRI—Magnetic resonance imaging is another imaging test that enables a detailed image of the organs. This test, however, is safe for pregnant individuals as it doesn’t involve X-rays.
- Ventilation-perfusion (V/Q) scan involves injecting a small amount of radioactive substance into a vein, which maps the blood flow and compares it to the lungs’ airflow.
Treatment
Treatment options include medications, surgery, and other medical procedures. Rapid treatment is essential to prevent complications and death.
Medications
Clot dissolvers are used in some cases of the condition. Small clots usually dissolve, and medications are used only to prevent them from getting more significant. However, when a clot is large and causes life-threatening symptoms, medicines that dissolve blood clots are given, usually directly into the lung artery. Those drugs are used only when necessary because they may cause severe bleeding.
If the condition doesn’t threaten life and the blockage is insignificant, treatment usually consists of blood thinners, preventing the clots from forming and growing. In this scenario, the body breaks the clot, blocking the lung artery, while medications prevent the condition from worsening. Blood thinners may be injected or taken orally, depending on the type.
Surgery
When someone has blood clots blocking their lungs, doctors might do surgery like:
- Taking out the clot – They can get rid of it by using a thin, bendable tube that goes through the veins.
- Putting in a vein filter—To prevent clots from blocking the lungs, doctors can insert a filter in a vein. This filter catches big clots before they can reach the lungs again. Using a filter does not cure thrombosis but only prevents its complications. Therefore, this method is used only when, despite treatment, lung blockage recurs or the administration of drugs used to treat thrombosis is impossible.
Prognosis
When pulmonary embolism is left untreated, it often leads to death. Experts estimate that around 30% of people with lung artery blockage die if left untreated. When treatment is implemented, the death rate drops to about 8%. If the treatment is delayed, it can lead to lung or heart damage.
Prevention
Preventing blood clots from developing and extending in your leg veins may prevent pulmonary embolism from happening. To achieve this, the following measures are used:
- Blood thinners – are often prescribed to people with conditions that are at risk of blood clot formation, such as cancer, heart attack, or DVT. If you are undergoing major surgery, your physician may prescribe blood thinners before and after the procedure to avoid blood clot formation.
- Physical activity—working muscles help blood in veins flow smoothly and prevent blood clots. That’s why healthcare professionals usually recommend moving as soon as possible after surgery.
- Leg elevation –when legs are elevated, gravity helps the blood flow upwards in leg veins. If you have problems with leg veins, you can try elevating the bottom of the bed at night.
- Compression stockings—compression stockings help the blood flow more efficiently. It’s important to wear them the right way. The most significant pressure should be at the ankle and gradually decrease upwards.
Complications
Pulmonary embolism can be a life-threatening condition and may lead to several complications, including:
- Arrhythmias (irregular heartbeat)
- Cardiac arrest, meaning sudden stop of heartbeat
- Pulmonary hypertension, which is a high pressure in the lungs
- Pleural effusion occurs when the fluid builds up in the space around the lungs
- Pulmonary infarction (death of the lung cells)
- Chronic embolic pulmonary hypertension – occurs when minor lung blockages develop over time.
When Should You See a Doctor?
Contact an emergency medical attention if you notice any disturbing symptoms that may suggest pulmonary embolism. Those include chest pain, sudden shortness of breath, coughing up blood, anxiety, and fainting. Pulmonary embolism can be a life threat and should be consulted with healthcare professionals as soon as possible.
If you have deep vein thrombosis, you can talk to your physician about possible safety measures to prevent PE, as thrombosis is the most significant risk factor.
Sources
- Bĕlohlávek J, Dytrych V, Linhart A. Pulmonary embolism, part I: Epidemiology, risk factors and risk stratification, pathophysiology, clinical presentation, diagnosis and nonthrombotic pulmonary embolism. Exp Clin Cardiol. 2013 Spring;18(2):129-38. PMID: 23940438; PMCID: PMC3718593.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3718593/ - Kaur K, Bhardwaj M, Kumar P, Singhal S, Singh T, Hooda S. Amniotic fluid embolism. J Anaesthesiol Clin Pharmacol. 2016 Apr-Jun;32(2):153-9. doi: 10.4103/0970-9185.173356. PMID: 27275041; PMCID: PMC4874066.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4874066/ - Huisman MV, Barco S, Cannegieter SC, Le Gal G, Konstantinides SV, Reitsma PH, Rodger M, Vonk Noordegraaf A, Klok FA. Pulmonary embolism. Nat Rev Dis Primers. 2018 May 17;4:18028. doi: 10.1038/nrdp.2018.28. PMID: 29770793.
https://pubmed.ncbi.nlm.nih.gov/29770793/ - Moore AJE, Wachsmann J, Chamarthy MR, Panjikaran L, Tanabe Y, Rajiah P. Imaging of acute pulmonary embolism: an update. Cardiovasc Diagn Ther. 2018 Jun;8(3):225-243. doi: 10.21037/cdt.2017.12.01. PMID: 30057872; PMCID: PMC6039809.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6039809/ - National Heart, Lung, and Blood Institute (NIH) What Is Pulmonary Hypertension? (2023)
https://www.nhlbi.nih.gov/health/pulmonary-hypertension - Abdol Razak NB, Jones G, Bhandari M, Berndt MC, Metharom P. Cancer-Associated Thrombosis: An Overview of Mechanisms, Risk Factors, and Treatment. Cancers (Basel). 2018 Oct 11;10(10):380. doi: 10.3390/cancers10100380. PMID: 30314362; PMCID: PMC6209883.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6209883/ - National Library of Health (NIH) Madhu Badireddy; Vasudeva Ranjit Mudipalli. Deep Venous Thrombosis Prophylaxis (2023)
https://www.ncbi.nlm.nih.gov/books/NBK534865/ - National Library of Health (NIH) Altif Muneeb; Amit S. Dhamoon. Inferior Vena Cava Filter (2023)
https://www.ncbi.nlm.nih.gov/books/NBK549900/