The manifestation of skin psoriasis often happens before arthritic symptoms appear. Surprisingly, it’s not just limited to affecting your skeleton. Other parts, like the eyes, can also be impacted. It also can speed up the progression of conditions like atherosclerosis and its accompanying complications.
The disease can have a very diverse course – from mild to severe forms, leading to joint destruction and disability.
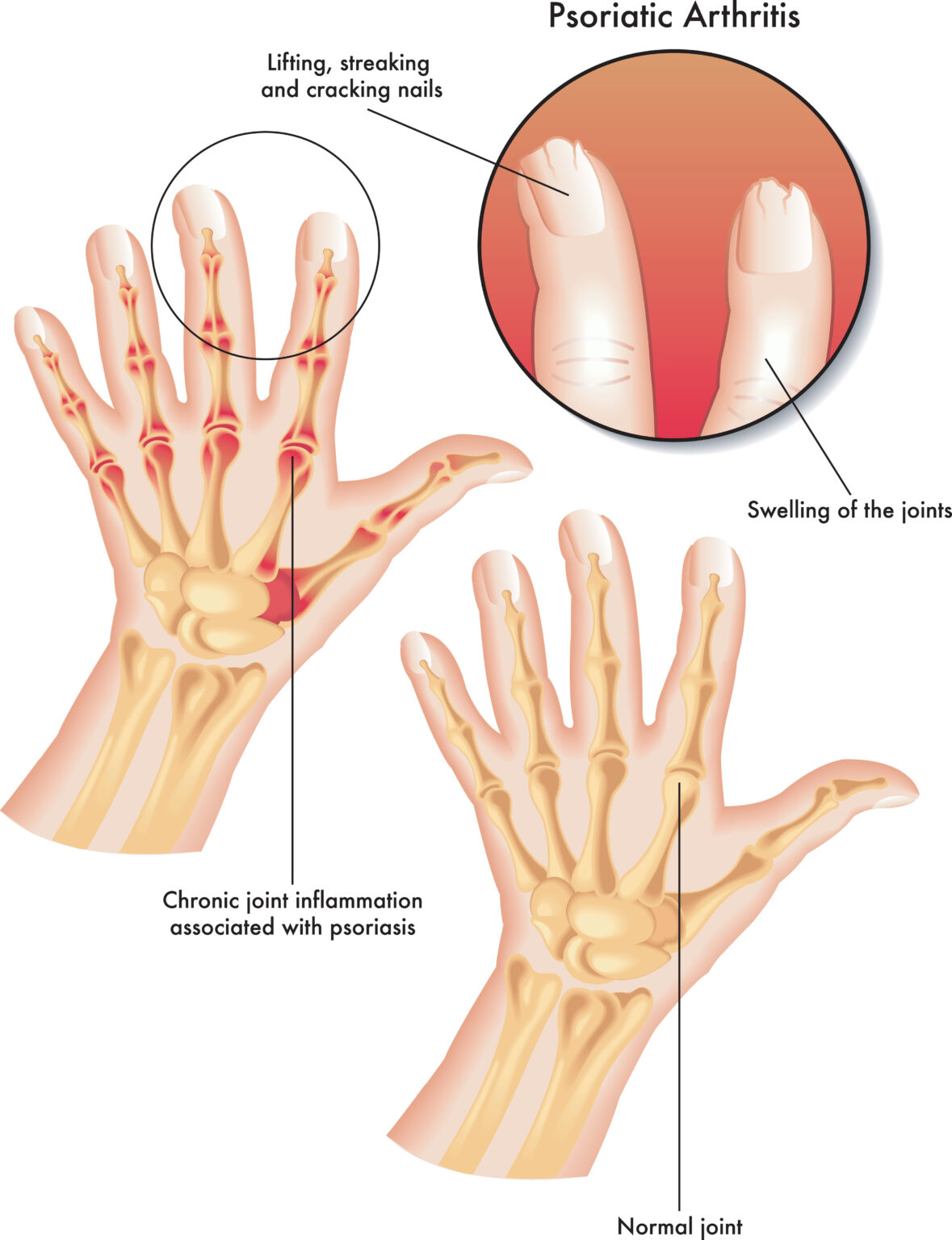
Psoriatic arthritis and psoriasis are autoimmune diseases. This means that, for some reason, the immune system overreacts and starts attacking the body’s cells. In psoriasis, skin inflammation causes the appearance of discolored skin patches covered with scales. As a result, these areas of skin are thicker and are called plaques. Also, the nails become more viscous and look pitted.
In most people with psoriatic arthritis, the disease occurs in periods of flare-ups and remission.
Causes
If you have psoriatic arthritis and psoriasis, your immune system starts attacking healthy cells and tissues. This causes joint inflammation and overproduction of skin cells. The exact cause of immune system overreaction is not known. An additional factor in people with a genetic predisposition likely triggers the abnormal inflammatory process. The triggering factors include:
- Viral and bacterial infections
- Injuries
- Severe stress
- Effects of some medications
- Certain chemical substances
How Common Is It?
Psoriatic arthritis affects around 1% of the population. Among people with psoriasis, PsA affects up to 40% of patients.
Risk Factors
Psoriatic arthritis most often occurs in people between 30 and 50. It affects men and women equally. However, it can affect anyone. Experts distinguish several risk factors that raise your chances of acquiring PsA. These include:
- Smoking
- Drinking too much alcohol
- Obesity
- Chronic stress
- Infections
Forms of Psoriatic Arthritis
There are five forms of psoriatic arthritis:
- Asymmetric Oligoarticular arthritis is the most common form (70%) that affects various joints asymmetrically on both sides of the body. Up to 5 joints are involved. In the beginning, these are most often the joints of the hands and feet.
- Symmetrical Polyarthritis: in this form, more than five joints are affected. Usually, it concerns wrists, hands, foot, and ankle joints. This form requires differentiation from rheumatoid arthritis because the joints are destroyed similarly.
- Inflammation of the distal interphalangeal joints (i.e., the end joints of the fingers and toes) occurs in approximately 10% of people with PsA. It is often combined with lesions on the nails.
- Spondylitis: Your spine is made up of 33 bones called vertebrae. This type of disease affects the joints between the vertebrae of the spine and the sacroiliac joints (connecting the spine with the pelvis). The characteristic symptoms are pain and stiffness in the spine. The signs are most severe at night and in the morning, and movement provides relief.
- Arthritis Mutilans: affects approximately 5% of sick people and causes significant destruction and deformation of joints. In this type, the inflammation is so intense that it leads to bone loss (osteolysis).
Symptoms
Psoriatic arthritis has a varied course, depending on the degree of involvement of the joints and other organs. It may manifest itself in only one location (e.g., as recurrent dactylitis) or affect many joints. Symptoms of psoriatic arthritis most often appear in people with already diagnosed psoriasis or simultaneously with skin lesions. However, sometimes psoriatic arthritis begins in people without skin symptoms of psoriasis, which sometimes poses a problem in making the diagnosis.
The disease usually has periods of flare-ups, followed by remission when symptoms disappear entirely or partially. General symptoms, such as fatigue, fever, or general malaise, usually accompany high disease activity.
The symptoms of psoriatic arthritis concerning the joints include:
- Arthralgia (joint pain)
- Stiffness and swelling of joints
- Limited joint mobility
- Redness or discoloration of the skin around the affected joints
- Inflammation of the attachment points of tendons and ligaments to the bones. It manifests with pain and tenderness in places such as the heels and the junction of the ribs with the sternum and the spine.
- Inflammation of the finger (dactylitis) – the disease affects all structures of the finger, which causes swelling and gives the characteristic symptom of a “sausage finger.” The affected finger is widened, painful, and red.
- Joint deformations – occur mainly in the form of arthritis mutilans.
Symptoms of Other Organs
Throughout the illness, various symptoms manifest in joints and concern other body organs and tissues. These include:
- Skin – Psoriatic arthritis is typically accompanied by skin psoriasis. Features like reddish patches adorned with a keratinized surface that mirrors silver scales are common signs. The size and coverage of the lesions can differ greatly, from tiny spots to nearly full-body outbreaks. It most often affects the head, elbow, knee, navel, and buttocks areas. The severity of skin lesions is not usually related to the severity of arthritis.
- Eyes are affected in approximately 10% of people with psoriatic arthritis. The most common condition is conjunctivitis. Less common is uveitis, manifesting in pain, eyeball redness, and vision problems. Untreated uveitis can lead to severe complications.
- Atherosclerosis – its accelerated development in psoriatic arthritis results from chronic inflammation. Complications of atherosclerosis, such as heart attack and stroke, are life-threatening, so it is essential to start preventing its development as soon as possible.
- Heart – rarely, the disease causes damage to the heart valves, inflammation of the aorta, or disturbances in the conduction of cardiac impulses. Patients should see a cardiologist if they experience symptoms such as chest pain, shortness of breath, physical weakness, or fainting.
- Nails – nail involvement occurs in 80% of patients with psoriatic arthritis (twice as often as in psoriasis). Characteristic lesions include nail pitting, transverse or longitudinal grooves, yellow spots, and peeling of the nail. Nail involvement, in some cases, may be the only symptom of psoriasis, so it should not be underestimated.

Diagnosis
If the doctor suspects psoriatic arthritis, they will ask you about the current and previous condition of your fingers, toes, and nails, such as onycholysis (your nail separating from the skin beneath it), nail pitting, and bleeding under your nails. The doctor will also ask about psoriasis symptoms and joint pain.
At your appointment, the physician will inspect your joints for signs of inflammation, such as redness, swelling, or pain. A comprehensive skin examination is also conducted to identify symptoms like reddened areas with silver scales, pus-filled blisters, or tiny crimson spots, which could signal psoriasis manifestations on the skin.
There is no specific test for psoriatic arthritis. However, your physician may still run some blood tests to exclude other medical conditions. They may check your blood for rheumatoid factor (RF) since one of the few features specific to PsA is the absence of rheumatoid factor distinguishing it from rheumatoid arthritis. To confirm the diagnosis of psoriatic arthritis, doctors mostly use the CASPAR criteria:
| Clinical feature | Points |
| Skin psoriasis (present/family history) | 2/1 |
| Nail lesions | 1 |
| Dactylitis (finger inflammation) | 1 |
| Absence of rheumatoid factor (RF) in the blood | 1 |
| Near-joint new bone formation | 1 |
Getting at least three points using this criteria confirms the diagnosis of psoriatic arthritis.
If the doctor suspects spondylitis form, they perform scans of the spine and sacroiliac joints. Ultrasound of the joints is also helpful in further assessment of the disease, as it allows for detecting signs of inflammation in the joints and tendons. Patients with symptoms of conjunctivitis or uveitis require an ophthalmological examination.
Treatment
The goal of treatment for psoriatic arthritis is to achieve remission. Moreover, the treatment of psoriatic arthritis is aimed at inhibiting further progression of the disease, which, over the years, may lead to the patient’s disability.
Medications
Anti-inflammatory drugs, including non-steroidal anti-inflammatory drugs (such as paracetamol) and corticosteroids, are used for treatment to fight the inflammation in the joints.
Drugs that suppress the immune system and disease-modifying medications are used in more severe forms of the disease.
It is crucial to start treatment as soon as possible to prevent disability and other complications of the disease. The treatment method depends on the course of psoriatic arthritis and must be adapted to each patient. The doctor will determine the treatment, taking into account the activity of the disease, the degree of damage to joints and other organs, and comorbidities.
In some people, joint aspiration, which is the removal of the fluid from the joint using a needle, might be necessary, and sometimes, when the disease destroys the joint, replacement surgery is performed.

Non-pharmacological Treatment
When treating psoriatic arthritis, apart from the use of drugs, other therapeutic methods are essential. These include:
- Mental support – patients with psoriatic arthritis often experience pain and discomfort, and an additional cause of their suffering is skin lesions. Being diagnosed with this disease can cause enormous stress and anxiety about the future. This is what most people suffering from a chronic illness struggle with, so it is vital to get help and support from loved ones and, if necessary, through therapy or support groups.
- Physical therapy – various techniques such as cryotherapy, ultrasound therapy, and massage help reduce joint pain and inflammation and relax the muscular system.
- A healthy diet – this is necessary to maintain adequate body weight. Patients should avoid being overweight (which increases the load on joints and accelerates the development of atherosclerosis) and malnutrition, which weakens the body and leads to muscle atrophy.
- Exercises – When dealing with joint disease, not abandoning movement and exercise is essential. Regular activity assists in combating a lack of flexibility in joints, muscle spasms, and loss of muscular strength. Engaging a physiotherapist is recommended for designing an appropriate workout schedule based on the impact level of condition, physical resilience, and other health circumstances unique to individual patients.
Psoriatic Arthritis and Pregnancy
If you have psoriatic arthritis and are planning a pregnancy, it is crucial to inform your doctor about it. Psoriatic arthritis is not a contraindication to having children, but pregnancy should be planned to modify the treatment early enough, as most drugs may harm the fetus.
Complications
People with psoriatic arthritis are likely to develop other medical conditions, such as:
- High cholesterol
- Dyslipidemia
- Atherosclerosis
- Diabetes
- High blood pressure
- Obesity
- Depression
Other psoriatic arthritis complications stem from decreased bodily movement. The discomfort in joints can make participating in workouts difficult. Hence, seeking medical assistance and starting treatments is vital to maintain mobility and avoid disease-related complications.
Prevention
Since the cause of immune system attacks on joints in PsA remains unknown, there is no specific way of preventing psoriatic arthritis. However, there are risk factors that have been proven to higher your chances of getting it, so avoiding it seems reasonable:
- Quit smoking
- Cut down on alcohol
- Avoid becoming obese by following a healthy diet
- Maintain low-impact regular physical activity, for example, swimming or yoga
- Avoid chronic stress and infections
Prognosis
Psoriatic arthritis is a chronic disease and, in most cases, lifelong. Quite often, however, it is mild, with long periods of remission.
Available treatment methods allow long periods of remission and normal functioning. Unfortunately, in some patients, the disease has an aggressive course and leads to severe joint deformations and disability.
When Should You See a Doctor?
If you have psoriasis, you should inform your doctor if you experience symptoms such as joint pain, swelling, stiffness, or redness of the skin around the joint – these may be the first symptoms of psoriatic arthritis. Joint pain and swelling require consultation with a rheumatologist to establish the diagnosis as early as possible and apply effective treatment.
If you have psoriatic arthritis, you should urgently contact your doctor if the symptoms worsen despite treatment or you experience symptoms such as eye pain, redness, or vision problems – these may be symptoms of uveitis requiring immediate ophthalmological treatment.
A rheumatologist treats people with psoriatic arthritis. However, patients are often also treated by a dermatologist and an ophthalmologist in case of skin lesions or ocular symptoms of the disease.
Sources
- National Library of Medicine (NIH) Vivekanand Tiwari; Lawrence H. Brent. Psoriatic Arthritis (2023) https://www.ncbi.nlm.nih.gov/books/NBK547710/
- National Health Service (NHS) Psoriatic Arthritis (2023) https://www.nhs.uk/conditions/psoriatic-arthritis/
- Constantin MM, Ciurduc MD, Bucur S, Olteanu R, Ionescu RA, Constantin T, Furtunescu F. Psoriasis beyond the skin: Ophthalmological changes (Review). Exp Ther Med. 2021 Sep;22(3):981. doi: 10.3892/etm.2021.10413. Epub 2021 Jul 12. PMID: 34345263; PMCID: PMC8311223. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8311223/
- Pala E, Melikoğlu M, Karaşahin Ö, Alkan Melikoğlu M. The Frequency of Association of Nail Involvement and Psoriatic Arthritis in Psoriasis Patients. Eurasian J Med. 2023 Jun;55(2):158-164. doi: 10.5152/eurasianjmed.2023.53. PMID: 37403914; PMCID: PMC10440947. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10440947/
- Zhu TY, Li EK, Tam LS. Cardiovascular risk in patients with psoriatic arthritis. Int J Rheumatol. 2012;2012:714321. doi: 10.1155/2012/714321. Epub 2012 May 8. PMID: 22645614; PMCID: PMC3356896. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3356896/
- Sudoł-Szopińska I, Matuszewska G, Kwiatkowska B, Pracoń G. Diagnostic imaging of psoriatic arthritis. Part I: etiopathogenesis, classifications and radiographic features. J Ultrason. 2016 Mar;16(64):65-77. doi: 10.15557/JoU.2016.0007. Epub 2016 Mar 29. PMID: 27104004; PMCID: PMC4834372. https://pubmed.ncbi.nlm.nih.gov/27104004/
- Sudoł-Szopińska I, Matuszewska G, Kwiatkowska B, Pracoń G. Diagnostic imaging of psoriatic arthritis. Part I: etiopathogenesis, classifications and radiographic features. J Ultrason. 2016 Mar;16(64):65-77. doi: 10.15557/JoU.2016.0007. Epub 2016 Mar 29. PMID: 27104004; PMCID: PMC4834372. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4834372/
- Girolimetto N, Giovannini I, Crepaldi G, De Marco G, Tinazzi I, Possemato N, Macchioni P, McConnell R, McGonagle D, Iagnocco A, Zabotti A. Psoriatic Dactylitis: Current Perspectives and New Insights in Ultrasonography and Magnetic Resonance Imaging. J Clin Med. 2021 Jun 12;10(12):2604. doi: 10.3390/jcm10122604. PMID: 34204773; PMCID: PMC8231617. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8231617/
- Ogdie A, Gelfand JM. Clinical Risk Factors for the Development of Psoriatic Arthritis Among Patients with Psoriasis: A Review of Available Evidence. Curr Rheumatol Rep. 2015 Oct;17(10):64. doi: 10.1007/s11926-015-0540-1. PMID: 26290111; PMCID: PMC5278907. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5278907/
- Kurizky PS, Ferreira Cde C, Nogueira LS, Mota LM. Treatment of psoriasis and psoriatic arthritis during pregnancy and breastfeeding. An Bras Dermatol. 2015 May-Jun;90(3):367-75. doi: 10.1590/abd1806-4841.20153113. PMID: 26131868; PMCID: PMC4516109. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4516109/
- Karmacharya P, Ogdie A, Eder L. Psoriatic arthritis and the association with cardiometabolic disease: a narrative review. Ther Adv Musculoskelet Dis. 2021 Mar 2;13:1759720X21998279. doi: 10.1177/1759720X21998279. PMID: 33737966; PMCID: PMC7934027. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7934027/