Inflammation affects one or more bones and joints. As a result of the inflammatory process, pus collects, which begins to spread through the vessels and leads to necrosis and disturbances in the nutrition of the skeleton.
During arthritis, pathological changes affect both its bone elements, cartilage, synovial membrane, and joint bursae. Arthritis may accompany osteomyelitis or occur alone.
In the osteoarticular system, depending on the disease factor causing the inflammatory process, we distinguish:
- Non-specific inflammations are most often bacterial, fungal, or viral. Microorganisms enter the bones through the bloodstream from other places with an active inflammatory process (e.g., from a lung abscess when the body’s defenses are weakened).
- Specific inflammations include osteoarticular tuberculosis, syphilis, and brucellosis.
In adults, it usually affects the pelvic bones or spine. The disease can appear at any age but is more common in children during the rapid body growth period, especially in boys. Bone inflammation affects the periosteum (tissue covering the bone), bone tissue, bone marrow, and joints. It may lead to permanent damage.

Causes
The causes of osteoarthritis include:
- Blood-borne infection with microorganisms (staphylococcus bacteria, tuberculosis bacilli, syphilis spirochetes, fungi, streptococci, influenza, and salmonella bacilli, in the case of joints – sometimes viruses)
- Metastases from primary infection sites such as umbilical cord, otitis media, pneumonia, or angina
- Infection as a result of injury (prick, bite, fracture, gunshot), surgical or dental procedure
- Use of intravenous drugs
- Repeated injuries
- Harmful effects of ionizing radiation
- Phosphorus poisoning
The following may predispose people to osteomyelitis:
- Decreased immunity
- Blood circulation disorders
- Systemic diseases (diabetes, lupus, systemic sclerosis, obesity, connective tissue diseases)
- Joint replacements
Symptoms
Symptoms of osteoarthritis include:
- Fever
- Spontaneous night pain
- Sensitivity of the area to touch
- Edema
- Reddening
- Warming of the infected area
- Impairment of joint function (stiffness and difficulty in movement)
- Formation of a skin fistula over the infected bone site
- General malaise (fatigue, weight loss, nausea, chills, muscle pain)
In small children, there may be a reluctance to move the affected limb, avoidance of walking, and crying when touching and moving the affected limb.
Diagnosis
In the case of purulent disease in bones and joints, it is particularly significant to start treatment quickly. If treatment is not started in time, the abscess may break through the skin, and there will be apparent improvement, but the process becomes chronic and challenging to treat.
Suspected osteomyelitis requires urgent consultation with an orthopedic doctor and diagnosis. The specialist must pay particular attention to the following:
- The occurrence of the above-mentioned symptoms of osteomyelitis, especially in children under fifteen years of age, diabetics, or elderly people.
- The appearance of purulent discharge from the fistula over the bone, fever, or severe pain during treatment of another bacterial disease.
If inflammation is suspected, the doctor will perform the following tests:
- General blood tests – inflammation is characterized by leukocytosis (increased level of white blood cells), accelerated ESR, increase in the so-called acute phase proteins (e.g. CRP), and decreased hemoglobin levels.
- Microbiological tests (culture) of blood to detect the bacteria that cause inflammation.
- Bacteriological examination of the inflammation site.
- Imaging tests: X-ray, computed tomography, and magnetic resonance imaging. The changes are visible only after two weeks of the disease. These are usually foci of bone necrosis, periosteal layering, and blurring of the trabecular structure of the bone.
When differentiating non-specific osteoarthritis, the doctor mainly considers bone cancers (e.g., Ewing’s tumor, osteosarcoma, chondrosarcoma) or bone tuberculosis.
Treatment
Non-pharmacological therapies are necessary for osteoarthritis and are supported by varying levels of evidence for safety and effectiveness. Such activities should first be tried or initiated simultaneously with pharmacotherapy. The therapist’s role in the non-pharmacological treatment of OA is to recognize the patient’s needs and immediately refer him to other specialists to ensure access to appropriate specialized ongoing care.
The most commonly used therapies include patient education to maintain independence, stationary and aquatic exercises, and a possible recommendation to control or significantly reduce body weight. In some cases, it is necessary to use orthopedic equipment, such as canes, walkers, or TENS equipment (transcutaneous electrical nerve stimulation). Corrective footwear can also relieve pain and improve function.

Patients seeking osteoarthritis therapy can also be referred to a dietitian, physiotherapist, or occupational therapist. TENS, acupuncture, heat or cold therapy, and massage have also been shown to reduce pain and stiffness in people with degenerative diseases, such as knee disease.
Treatment of the disease is challenging due to poor penetration of the antibiotic administered systemically to the site of inflammation. If we help antibiotics within three days of the onset of inflammation, the disease can be fully cured. After this time, treatment is usually unable to stop the changes occurring in the bone. Therefore, it is necessary to diagnose and implement appropriate treatment quickly. Diagnosis of the disease usually requires hospitalization.
The primary medicine is antibiotics, which are mainly administered intravenously. Nowadays, modern antibiotics can be administered orally or by intramuscular injection. Antibiotics are used long-term, sometimes even for 8-10 weeks. There is usually a need to use painkillers. Proper diet, hydration, and bed rest are also essential.
The patient should exercise with healthy limbs, especially during a longer hospital stay. During treatment, surgical intervention is often necessary. In infants, this involves incising the subperiosteal abscess and draining the pus. In older children and adults, a wide opening of the bones and joints is performed, as well as the removal of pus, soft tissue fragments, necrosis, abundant irrigation of the wound, and local administration of an antibiotic. After surgery, the limb must be immobilized.
Complications
Possible complications of the disease include:
- Abscess and purulent fistula on the skin. The formation of a fistula is usually associated with a decrease in pain and fever. However, this is not a sign of improvement because it predisposes the disease to the chronic phase.
- Fracture of an inflamed bone.
- Cartilage damage.
- Epiphysis and, as a result, bone deformation and bending.
- Stiffness of surrounding joints and contractures.
- A long-term purulent process leads to the formation of amyloidosis.
- Septicemia and the formation of distant abscesses also in other bones.
- Bone defects and the formation of pseudoarthrosis.
- Amputation of a limb results from impaired blood circulation in the limb.
Osteoarthritis is the most common bone and joint inflammation, accounting for approximately 70% of cases. It is one of the most dangerous complications of musculoskeletal injuries, often leading to irreversible damage to the bones and surrounding soft tissues and then to the entire limb. It can also cause damage to many other organs and systemic disorders. Pathogenic bacteria penetrate the bones due to injuries sustained during open fractures and after orthopedic procedures on the osteoarticular system.
Post-traumatic Osteomyelitis – Risk Factors
It is one of the forms of hematogenous osteomyelitis located in the area of the metaphyses of long bones. It occurs when the patient’s immunity is high, and the bacteria-causing infections are less virulent. The focus of infection is usually tiny and is separated from healthy tissue by a fibrous capsule, preventing fistula formation. Locally, the disease manifests through swelling, soreness, and crushing pain, especially at night. Usually, the radiological image is characteristic and sufficient to diagnose the condition.
Factors contributing to post-traumatic osteomyelitis are:
- Immunodeficiency
- Extent and depth of damage
- Extensive post-traumatic hematoma
- Open fractures
- Poor wound dressing
- Surgical technique errors
- Impaired blood supply
Treatment involves the removal of infected tissues, external stabilization, and intensive general and local antibiotic therapy. Soft tissue and bone defects are covered with autogenous grafts (coming from the patient himself).
Other Types of Arthritis
There are over 100 kinds of arthritis, but only a few are the most ordinary. The causes of their occurrence are not entirely clear, but it is assumed that most of them are autoimmune diseases (caused by the body’s autoimmunity).
Osteoarthritis
As mentioned before, OA is one of the diseases that cause the most severe disability. It is the most common type of arthritis. A disturbance in the quantity and quality of articular cartilage causes it. It is a chronic disease leading to the degradation of all joint tissues: as the disease progresses, the articular cartilage becomes harder, thinner, and loses elasticity, the joint capsule and periarticular ligaments become thickened and less and less flexible, cysts form in the epiphyses of the bones, and on the border of the cartilage and bones develop osteophytes (bone growths).

Rheumatoid Arthritis (RA)
It is the second most popular type. The first symptoms of rheumatoid arthritis appear between the ages of 40 and 55, in most cases in women. Although the causes of the disease are not fully known, a significant role is attributed to the body’s autoimmunity and genetic factors.
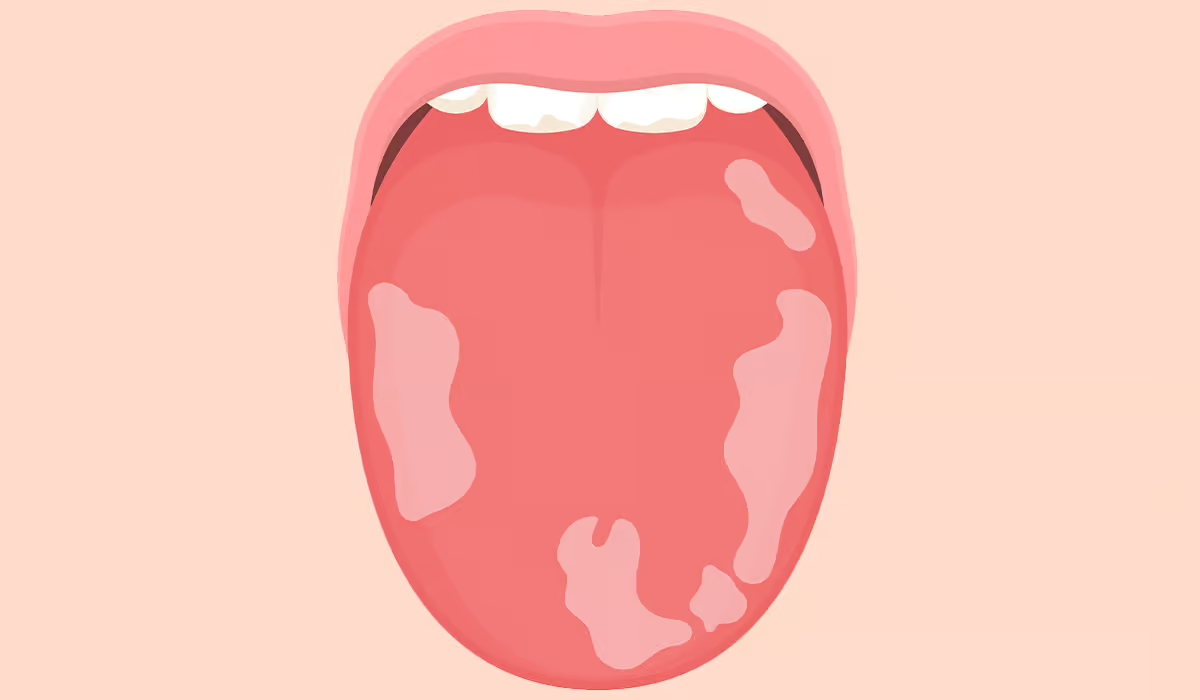
RA is characterized by non-specific inflammation of the symmetrical joints of the hands and feet (but also of large joints, e.g., hips or knees, but much less frequently). In addition to the symptoms typical of arthritis, there are also so-called rheumatoid nodules over the joints (mainly around the elbows). In the case of RA, finger degeneration and the formation of the so-called “swan necks”, almost entirely prevent normal functioning – the patient has difficulty grasping small objects in his hands (e.g., a pen).
Juvenile Idiopathic Arthritis (JIA)
Juvenile idiopathic arthritis, otherwise known as juvenile rheumatoid arthritis, is a chronic connective tissue disease that can cause damage not only to joints but also to muscles, skin, bones, tendons, and even eyes, lungs, digestive tract, heart, and blood vessels. This type of arthritis occurs before age 16 and is the most common type of inflammatory rheumatic disease in children. The duration of inflammation is six weeks or longer. As a consequence of the disease, growth disturbances, the occurrence of rheumatoid arthritis, and disability with multi-joint degeneration in adulthood, as well as a shortened life expectancy, are possible.
Gout
This disease is caused by uric acid precipitating calcium oxalate crystals in the synovial fluid. These crystals irritate the joint structure, which leads to inflammation. An attack of this condition usually occurs after an extensive and fatty meal or alcohol consumption and develops within a few hours. Characteristic gout symptoms are severe pain, redness, warmth, and limited movement of one joint (often, it is the big toe, but the disease can occur in any joint). Moreover, high levels of uric acid in the blood hurt the circulatory system and are associated with the risk of death from cardiovascular causes.
Systemic Lupus Erythematosus (SLE)
Systemic or isolated lupus erythematosus is an inflammatory disease of connective tissue that damages many organs and tissues, including joints, skin, kidneys, heart and blood vessels, and the peripheral and central nervous system. The causes of the disease are unknown. The disease often affects young people and usually does not manifest itself immediately – it is often diagnosed only after several years. Delayed detection and implementation of appropriate treatment contribute to the deterioration of the quality of life and even threat to the patient’s life.
Spondyloarthropathies (SpA)
These are arthritis affecting the joints of the spine. It most often occurs after the age of 40. Characteristic symptoms include spine and back pain that appears at night and during the day and improves after getting out of bed or exercises but does not improve after resting. In the course of these diseases, osteophytes may form. The following spondyloarthropathies include:
- Ankylosing spondylitis (AS)
- Reactive arthritis (Rea)
- Psoriatic arthritis (PsA)
- Arthritis that accompanies inflammatory bowel diseases, e.g., Crohn’s disease, ulcerative colitis
Septic arthritis
Septic arthritis is a chronic or acute inflammation of the joints that occurs when microorganisms get into the synovium.
Inflammation Caused by Infection
It occurs as a complication after an infection. The most common inflammatory conditions after illness are rheumatic fever (strep throat) and Lyme disease. Joint problems also often occur after viral infections in young children.
Sources
- Osteoarthritis. NIH. https://www.niams.nih.gov/health-topics/osteoarthritis.
- Osteomyelitis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK532250/.
- Osteoarthritis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK482326/.
- Osteoarthritis: symptoms, signs and source of pain. NIH. https://pubmed.ncbi.nlm.nih.gov/15035776/.
- Osteoarthritis Basics: Diagnosis, Treatment, and Steps to Take. NIH. https://www.niams.nih.gov/health-topics/osteoarthritis/basics/diagnosis-treatment-and-steps-to-take.
- Osteoarthritis complications and the recent therapeutic approaches. NIH. https://pubmed.ncbi.nlm.nih.gov/34755232/.
- Non-pharmacological therapies in osteoarthritis. NIH. https://pubmed.ncbi.nlm.nih.gov/9429737/.
- Role of D*********e as an Osteoarthritis Disease-Modifying Drug. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10145123/.
- Osteoarthritis and risk of hospitalization for ambulatory care-sensitive conditions: a general population-based cohort study. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8410004/.
- Treatment and support. NHS. https://www.nhs.uk/conditions/osteoarthritis/treatment/.
- Exercise and osteoarthritis: an update. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6165969/.
- Post-traumatic osteomyelitis. Pathophysiology and management. NIH. https://pubmed.ncbi.nlm.nih.gov/2643936/.
- Arthritis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK518992/.
- Rheumatoid Arthritis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK441999/.
- Juvenile Idiopathic Arthritis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK554605/.
- Gout. NIH. https://www.ncbi.nlm.nih.gov/books/NBK546606/.
- Systemic Lupus Erythematosus. NIH. https://www.ncbi.nlm.nih.gov/books/NBK535405/.
- Spondyloarthropathies. NIH. https://pubmed.ncbi.nlm.nih.gov/22424199/.
- Septic Arthritis. NIH. https://www.ncbi.nlm.nih.gov/books/NBK538176/.