On the other hand, the spinal cord aids in transmitting nerve impulses between the brain and the peripheral nervous system, enabling conscious movement, coordination, balance control, muscle tension, and sensation of touch, pressure, and pain. Diseases affecting the central nervous system can result from e.g. impaired blood flow, infections, injuries, and congenital or acquired neurodegenerative diseases.
The peripheral nervous system comprises nerves and ganglia, which transmit information between the central nervous system and individual organs. Diseases of the peripheral nervous system are typically acquired, often due to conditions like diabetes, nutrient deficiencies, injuries, and alcohol abuse. These conditions can lead to sensory disorders, paresis, paralysis, and muscle atrophy.
The cornerstone of diagnosing and treating these disorders involves interviewing the patient and conducting a neurological examination.

Diseases
The diseases most frequently treated by a neurologist include:
- Migraine
- Cluster headache
- Continuous and paroxysmal hemicrania
- Drug-induced headaches
- Pain in the lumbar spine
- Sciatica
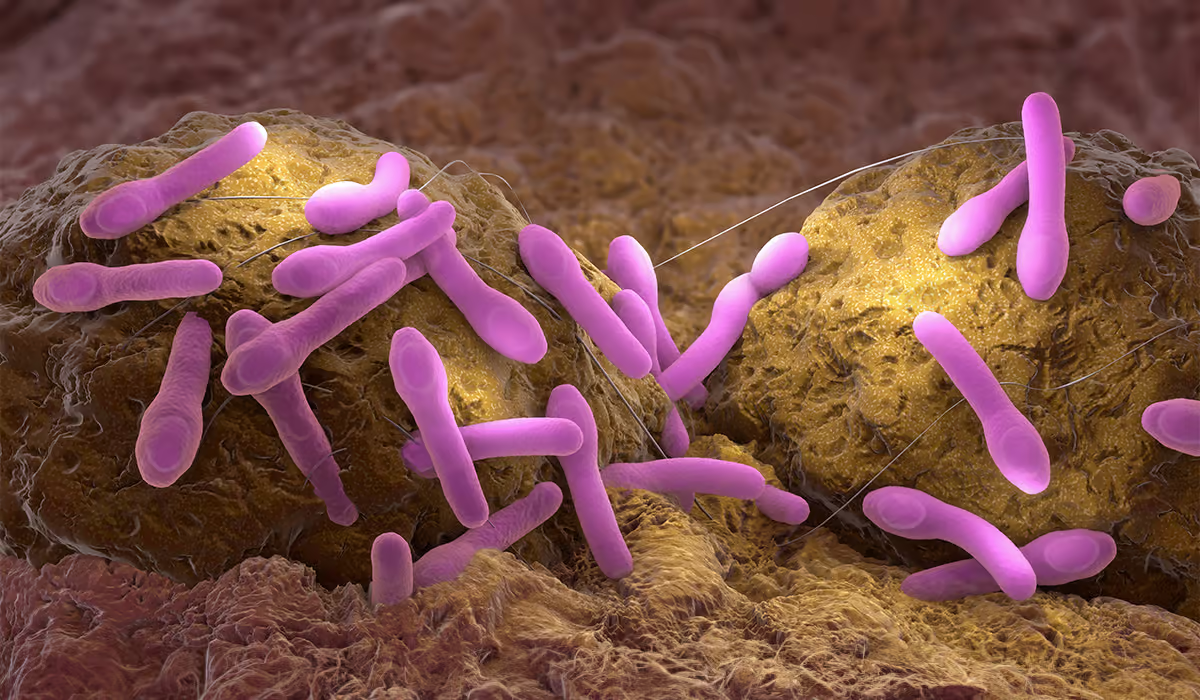
- Viral or bacterial meningitis
- Tick-borne encephalitis
- Mycoses of the central nervous system
- Vascular diseases
- Stroke
- Transient ischemic attack (TIA)
- Huntington’s chorea
- Parkinson’s disease
- Alzheimer’s disease
- Frontotemporal dementia
- Multiple sclerosis
- Guillain-Barré syndrome
- Amyotrophic lateral sclerosis
- Spinal muscular atrophy (SMA)
- Polyneuropathy
- Epilepsy
- Myasthenia gravis
- Tourette’s syndrome
- Craniocerebral injuries
- Concussion
Tests
Before running specific tests, the neurologist conducts a detailed medical interview with the patient. This interview aims to learn about the patient’s past neurological diseases, which may help determine which tests are needed. Before making a diagnosis, the neurologist performs or orders neurological tests, including functional, physical, vascular, and imaging tests.
Functional Tests
EEG (electroencephalogram) is necessary to assess the electrical activity of the brain, which is irreplaceable for making a diagnosis in cases in which the doctor suspects the occurrence of:
- Brain tumor
- Epilepsy
- Sleep disorders
- Poison with specific substances
An EMG test is used when a doctor assesses the electrical activity of muscles and peripheral nerves. This examination is used to diagnose:
- Muscular dystrophy
- Chronic discopathy
- Amyotrophic lateral sclerosis
- Carpal tunnel syndrome
Physical Examinations
Examination of the limbs and chest is performed to assess physiological reflexes, which include:
- Knees
- Thigh adductor muscles
- Biceps or triceps muscles
Vascular Tests
Doppler ultrasound of intracerebral arteries – blood flow in the intracerebral veins and arteries is determined by observing the wavelength of the ultrasound wave. This method is used to diagnose diseases such as:
- Frequent fainting
- Atherosclerosis
- Condition after ischemic stroke
- Occurrence of regular dizziness
Imaging Tests
Computed tomography is based on X-rays, enabling the detection of abnormalities in, among others, the brain or spine. Magnetic resonance imaging uses a magnetic field to diagnose diseases such as:
- Alzheimer’s disease
- Spinal canal tumors
- Brain tumors
- Multiple sclerosis
- Neurological disorders
Thanks to X-rays, the doctor can detect changes, among others within:
- Skulls
- Spine

Visit
A visit to a neurologist is similar to other visits to specialists. However, it requires appropriate preparation. The patient needs to keep a diary noting the symptoms and associated ailments. The more detailed and specific the description, the greater the chance for an accurate diagnosis during the visit and appropriately selected pharmacology. It is worth including the following information in the diary regarding:
- Diet and menu
- Sleep duration on a given day
- Physical exertion, including excessive exertion
- Weather changes or changes in atmospheric pressure
- Menstruation and cycle
- Hypersensitivity of the body to stimuli, e.g., strong odors
- Type, duration, location, and intensity of pain
- Comorbidities
- Stress
- Symptoms accompanying migraine attacks and preceding the attack
- Medications you take
Consider starting a diary before your neurologist appointment. The more details you include, the better your chances of an accurate diagnosis and proper treatment. Also, think about potential questions for the specialist. Don’t forget to bring all your current medical records, such as blood tests, ESR, and cholesterol levels.
Visits Course
When you first meet with the neurologist, you are in for a thorough medical interview. The doctor may ask about your medications, symptoms, past illnesses, and family history of neurological diseases. Your lifestyle, job, and diet may also be discussed. This information helps the doctor form a complete understanding and aids in making an accurate diagnosis.
Following the interview, the neurologist will move on to a basic nervous system examination. It usually involves testing physiological reflexes like the biceps, knee, ankle, and brachioradial reflexes. The specialist will also assess speech, sensation, body posture, and walking patterns. Often, the interview and examination are enough for a diagnosis. If there’s any uncertainty, the neurologist may recommend additional neurological tests.
When Should I Go?
If you notice repeating neurological symptoms, seeing a neurologist as soon as possible is important. The first time the symptoms occur might go unnoticed, but if they return regularly, it’s a clear sign to get medical help. Neurological symptoms that the patient should not underestimate include:
- Insomnia
- Numbness and tingling in the limbs
- Convulsions
- Recurrent pain in various parts of the body
- Paresis
- Fainting
- Muscle weakness
- Memory deterioration
- Decreased vision
- Problems with concentration
- Issues with maintaining balance
- Muscle cramps
- Muscle stiffness
- Tics
- Loss of consciousness
- Occurrence of sensory disorders
- Motor coordination disorders
- Dizziness
Symptoms Requiring Urgent Intervention By A Neurologist
There are emergencies and unexpected symptoms that we cannot ignore in any way. Immediate intervention by a neurologist may save the patient’s life and health. Disturbing symptoms that should be immediately consulted with a neurologist include:
- Aggression
- Gibberish statements
- Involuntary movements
- Paresis or weakness of limbs occurring on one side of the body
- Inability to coordinate movements
- Persistent and severe headache
- Hallucinations
- Weakness of facial muscles, manifested by drooping of one corner of the mouth
- Paralysis
- Confusion consists of the inability to determine where and when the patient is
- Anxiety
- Delusions
- Loss of consciousness
- Blurred vision
Pediatric Neurology
Sometimes, a neonatologist, pediatrician, or family doctor may recommend a newborn or infant to see a pediatric neurologist for a preventive visit. It might be necessary if the baby was part of a high-risk pregnancy, born from a cesarean section, exposed to infections during pregnancy, or born prematurely with low birth weight. Since infants develop rapidly, it’s significant to closely monitor their developmental milestones – skills acquired in a particular order and time. All disturbing symptoms or possible delays should be reported to the pediatrician or family doctor, especially:
- Body asymmetry after the 3rd month of life – twisting of the body or lying on only one side, visible flattening of the head on one side, using only one hand
- Abnormal muscle tone, e.g., limpness, excessive tension, pulling the body back, clenching fists
- Stopping the child’s development, loss of already acquired skills
- Eyes wandering, lack of interest in the surroundings, and lack of eye contact
- Convulsions
Neurological symptoms in older children and teenagers may resemble those in adults. Particular attention should be paid to:
- Convulsions, hand tremors, and tics (epilepsy is one of the most frequently diagnosed neurological disorders in children and adolescents)
- Repeated fainting
- Symptoms of neurotic disorders – mood swings, hysteria, anger attacks, hyperactivity, aggression
- Speech problems, e.g., stuttering
- Recurring headaches
- Issues with concentration or memory
A neurological consultation may also be indicated when diagnosing ADHD or autism spectrum disorders.

Neurological Rehabilitation
Neurological rehabilitation is a process, a series of activities optimizing a person’s participation and functioning in society. It also involves restoring the highest possible quality of life. Rehabilitation in neurological diseases should not be treated as a special type of intervention, and attention must be focused on the patient as a person when selecting actions. Formulated short—and long-term goals should be based on social functioning, functional efficiency, and the psychological sphere.
Rehabilitation and physiotherapy in neurology should not cover all patients, not only those with good prospects.
Indications
Early neurological rehabilitation is almost a guarantee of improved functional efficiency. It is the main component of treatment for many different diseases. The basic indications for the use of neurological rehabilitation and exercises include:
- Condition after brain tumor surgery
- Parkinson’s disease
- Multiple sclerosis
- Condition after stroke
- Condition after craniocerebral trauma
- Down syndrome
- Polyneuropathy
- Bell’s facial nerve palsy
- Cerebral palsy
- Multiple disabilities
- Brown-Sequard syndrome
- Spinal muscular atrophy (SMA)
Neurological rehabilitation methods include a wide repertoire of concepts that provide opportunities to regain fitness. It is essential to know the indications for their use and to carry out rehabilitation procedures by applicable rules and only by qualified people.
Main Assumptions
Neurological rehabilitation is divided into early and chronic stages, with the selection depending on the specific disease presented. To ensure effectiveness, it requires a multidisciplinary team, including physiotherapists, psychologists, neurologists, and rehabilitation doctors. Early intervention has been shown to help complete recovery or reduce negative effects. Specialized facilities offering comprehensive assistance in rehabilitation activities are available for conditions like Parkinson’s disease, multiple sclerosis, stroke recovery, craniocerebral injury, cerebral palsy, and neurosurgical patients.
Physiotherapy Methods
Neurorehabilitation can occur in a rehabilitator’s office, where the exercises are discussed thoroughly with the patient. The rehabilitator may then prescribe exercises to be performed independently at home. Some patients may also opt for rehabilitation centers that provide comprehensive support in the neurorehabilitation process. The following are the most commonly used methods in neurorehabilitation:
- Vojta method – it focuses on improving movement and is known as reflex locomotion therapy. It involves manually stimulating pressure points using specific direction and force to create motor patterns. It is commonly used in the neurorehabilitation of children and can be effective in treating adults with conditions such as paralysis of peripheral nerves, cerebral palsy, muscular dystrophies, spinal cord injuries, hip dysplasia, and congenital brain defects
- Sensory integration therapy – this therapy aims to reorganize the sensory processing system through stimulation of the senses using various sensory stimuli. It is designed to address neurological deficits responsible for sensory processing disorders and integrate sensory processing to develop complex cognitive processes. Specialized equipment like balance beams, cushions, weighted vests, suspended platforms, swings, and materials of different textures are used for this therapy
- PNF therapy – proprioceptive neuromuscular facilitation of movement is used to reestablish correct movement patterns. The exercises mimic the natural way muscles and joints work and involve multi-sensory stimulation. PNF is beneficial for people with nervous system disorders, as well as osteoarticular and muscular issues
- The Bobath method – this whole-body exercise method focuses on regulating muscle tension and developing proper reflexes through motor learning, which involves teaching through movement
- Orthopedic accessories – various types of orthoses, corsets, stiffening vests, hip abduction devices, standing frames, and seats also play an important role in neurorehabilitation
- Psychotherapy and speech therapy – neurorehabilitation also includes psychotherapy, which focuses on eliminating the patient’s psychological barriers. The most frequently used method is cognitive-behavioral therapy, which teaches a new way of looking at yourself or a given situation. Speech therapy, in turn, aims to develop, shape and improve speech
Sources
- Neurologist. NHS.
https://www.healthcareers.nhs.uk/explore-roles/doctors/roles-doctors/medicine/neurology - Electroencephalogram. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK563295/ - What is an EMG/Nerve Conduction Study?. NHS.
https://www.sth.nhs.uk/clientfiles/File/EMG%20NERVE%20COND%20Test%20PD3061-PIL969v3.pdf - Neurologic Exam. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK557589/ - Transcranial doppler ultrasound (TCD). NHS.
https://www.newcastle-hospitals.nhs.uk/services/neurosciences/neuroradiology/transcranial-doppler-ultrasound-tcd/ - Computed tomography (CT). NHS.
https://www.uclh.nhs.uk/our-services/find-service/neurology-and-neurosurgery/neuroradiology/computed-tomography-ct - Children’s neurology. NHS.
https://www.imperial.nhs.uk/our-services/childrens-services/childrens-neurology - Neurorehabilitation. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3863977/ - Effects of Vojta Therapy on the Motor Function of Children with Neuromotor Disorders: Study Protocol for a Randomized Controlled Trial. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10707081/ - Sensory Integration. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK559155/ - Proprioceptive Neuromuscular Facilitation (PNF): Its Mechanisms and Effects on Range of Motion and Muscular Function. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3588663/ - The Bobath concept – a model to illustrate clinical practice. NIH.
https://pubmed.ncbi.nlm.nih.gov/29250987/ - What are some types of assistive devices and how are they used?. NIH.
https://www.nichd.nih.gov/health/topics/rehabtech/conditioninfo/device - Neuroscience-based psychotherapy: A position paper. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9968886/ - In brief: What is speech therapy?. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK561506/