Types
Various types of miscarriage can be identified based on the symptoms and changes in the uterus. These include, for example:
- Threatened miscarriage – this type is characterized by painless bleeding and mild uterine contractions. A gynecological examination may reveal a formed vaginal part of the cervix, moderate uterine bleeding, and an enlarged, sometimes tense uterus.
- Incomplete miscarriage – in this case, there is both pain and bleeding from the uterus. A gynecological examination may confirm a shortened cervix and the opening of the internal cervix, with elements of the fetal egg possibly visible.
- Complete miscarriage – this occurs when the fetus remains in the uterine cavity for more than eight weeks following its death. Symptoms include the lack of uterine enlargement for several weeks and the absence of fetal heart activity during an ultrasound examination.
It is also worth mentioning here that at least three consecutive miscarriages are called habitual miscarriages. There is also the term spontaneous miscarriage – it means that the pregnancy ends spontaneously without external intervention, medical intervention, trauma, taking medications, or pharmacological abortion. Spontaneous miscarriage is a term that often appears in the definition that miscarriage is the spontaneous termination of pregnancy.
Symptoms
The symptoms of miscarriage vary widely, and the gestational age plays a crucial role in determining its nature. The severity of these symptoms is also influenced by the stage of miscarriage, with more intense symptoms indicating a poor prognosis. It is only through a comprehensive analysis of the symptoms by a qualified medical professional that the risk to the pregnancy and the type of miscarriage can be accurately determined.
Vaginal Bleeding
Spotting or light bleeding, particularly during the first trimester of pregnancy, is generally not a cause for significant concern. However, miscarriage usually starts with bleeding. The bleeding may increase over several hours to several days and may be heavy for a short period. The embryo is expelled as clots and tissue debris (loss of uterine mucus).
Uterine Contractions
If atypical discharge or bleeding is coupled with uterine contractions, mainly if they are both painful and regular, it may indicate symptoms of a miscarriage. However, abdominal hardening, itching, or tingling symptoms are typically associated with prenatal contractions, which are preparatory uterine exercises before labor.
Abdominal Pain
Lower abdominal pain during pregnancy should always be taken seriously. Uterine pain, which is initially located below the navel and later expands upwards towards the ribs, can indicate a potential threat to the pregnancy. Symptoms such as pulling in the groin, tingling, feeling of pressure, or pressure on the perineum are typical at the end of pregnancy and do not necessarily indicate a cause for concern regarding miscarriage.
Unusual Symptoms
In the early stages of pregnancy, a sudden cessation of symptoms, such as nausea and fatigue, can be indicative of a potential loss of the pregnancy, mainly between 6 and 10 weeks. These symptoms typically begin to subside around the 8th week and become notably weaker after the 10th week, often disappearing entirely by the 12th week. Women who experience anxiety during the early stages of pregnancy may consider undergoing an ultrasound examination for reassurance.

Causes
In cases of miscarriage, the identification of causative factors often necessitates the undertaking of intricate genetic, immunological, and, at times, hormonal tests. While a singular miscarriage can occur in any woman, recurrent occurrences warrant a thorough investigation, including the examination of the aborted fetus. Typically, this process commences with screening for prevalent genetic anomalies.
Genetic Factors
Genetic mutations, encompassing both changes in the number of chromosomes and structural abnormalities, are a significant causative factor for miscarriages. These mutations may be inherited from one, or both parents, and recurrent miscarriages can often be attributed to genetic abnormalities present in the parental genetic code. In the majority of cases, genetic abnormalities are identified as the leading cause of miscarriages.
Corpus Luteum Failure
The corpus luteum, derived from the ovarian follicle, is crucial in producing progesterone, a hormone essential for preparing the uterine lining to receive the embryo during implantation. Progesterone also supports the early stages of pregnancy. Insufficient progesterone, stemming from corpus luteum dysfunction, can hinder embryo implantation. Additionally, progesterone is integral to preparing the uterine lining for implantation.
Anatomical Abnormalities
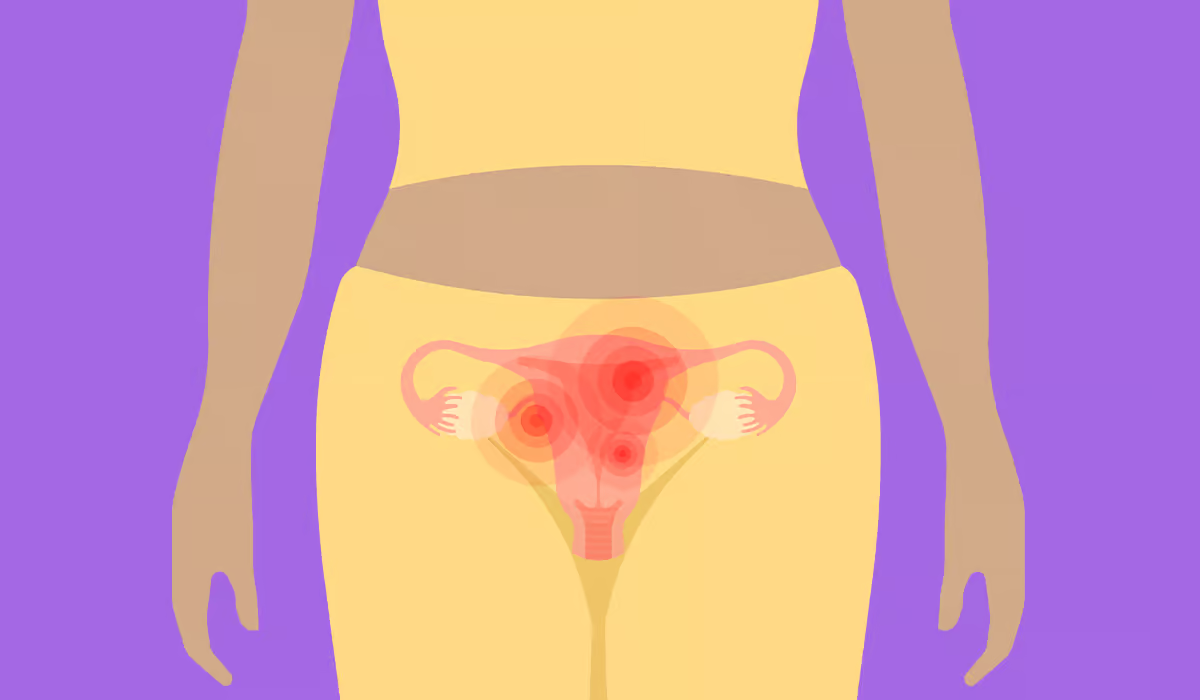
Another factor influencing the occurrence of miscarriages is anatomical defects. Anatomical factors that may predispose to miscarriage include:
- Defects such as a bicornuate uterus or a septate uterus – these defects may hinder the implantation of the embryo
- Adhesions within the uterine cavity (such adhesions may arise, among others, as a result of curettage of the uterus)
- Uterine fibroids
- Pelvic endometriosis – endometriosis is the presence of the uterine mucosa outside its natural place of occurrence, i.e. outside the uterine cavity
Autoimmune Diseases
Immunological factors are known to play a significant role in the pathogenesis of miscarriages. Notably, the antiphospholipid syndrome is a condition worth discussing in this context. This autoimmune disease is characterized by antiphospholipid antibodies in the body, recurrent miscarriages, reduced platelet count, and an inclination toward blood clot formation.
The presence of antiphospholipid antibodies increases not only the risk of miscarriage but also the risk of other obstetric complications, which include:
- Pregnancy-induced hypertension
- Premature separation of the placenta
- Intrauterine fetal growth restriction
Drug therapy is commonly employed in the management of women presenting with antiphospholipid antibodies and experiencing recurrent miscarriages.
Age Factor
As a woman’s age advances during pregnancy, the likelihood of experiencing a miscarriage rises. It is widely accepted that advanced maternal age is associated with an increased risk of genetic abnormalities in the fetus, consequently elevating the risk of miscarriage. Additionally, scientific literature indicates that older women have lower-quality egg cells or oocytes.
Infections
Some infections increase the risk of miscarriage. Infectious factors that increase this risk include:
- Rubella virus, cytomegalovirus, and herpes virus
- Measles virus – if the infection caused by this virus is accompanied by high fever, it is an essential risk factor for miscarriage.
- Toxoplasma gondii – a protozoan responsible for the development of toxoplasmosis. Congenital toxoplasmosis is associated with severe defects, including microcephaly, retinitis, and choroiditis. Infection of the fetus with this protozoan also increases the risk of miscarriage.
- Bacteremia – i.e., the presence of bacteria in the blood of a pregnant woman – toxins produced by bacteria can penetrate the placenta and lead to fetal death and miscarriage.
It is worth being aware that regardless of the pathogenic factor (i.e., virus or bacteria), the fever itself predisposes to the initiation of uterine contractions, which favors miscarriage.
Risk Factors During Pregnancy
It is pertinent to address prognostic factors that influence the course of pregnancy and significantly impact the risk of miscarriage. These factors primarily include:
- Gestational sac location – follicles positioned above the internal opening of the cervix are more predisposed to miscarriage compared to those situated at the bottom of the uterus. Ultrasound examination can determine the location of the gestational sac.
- Fetal heart rate – diminished fetal heart rate, known medically as bradycardia, serves as an adverse prognostic indicator.
- Uterine cavity bleeding – bleeding lasting four days or more is an unfavorable prognostic factor.
- Mothers lifestyle (e.g., obesity, drug or alcohol addiction, and history of miscarriages)
How To Recognize The Beginning Of A Miscarriage?
The signs of an impending miscarriage may initially be inconspicuous. The expulsion of a nonviable embryo from the woman’s body is indicative of this event. While the fertilized cell may reach the uterine cavity, the embryo’s viability may be compromised due to medical reasons, resulting in a miscarriage. This condition manifests through various symptoms.
Bleeding and spotting from the genital tract are the most common symptoms. Sometimes, even minor spotting may indicate a miscarriage, so even such a minor symptom should not be underestimated. Sometimes, this blood contains clots and tissue fragments. Many women often notice white-pink mucus or just watery discharge.
Abdominal cramps are a natural part of pregnancy – but only mild and transient ones should not cause any concern. Very often, contractions appear already at the embryo implantation stage. All abdominal pain, if it becomes more severe and lasts for a long time, may indicate a miscarriage.
Pain in the lower abdomen often appears together with pain in the lower back, quite intensely, and may signal any miscarriage.
In the first months of pregnancy, weight loss is rather typical for future mothers, and if it is small and systematic, it does not raise any suspicions. However, excessive and too rapid weight loss should worry every pregnant woman.
Specific ailments are characteristic of pregnancy, but the too-rapid loss of symptoms, such as breast tenderness or a sudden cessation of nausea, are indications that may also mean a miscarriage.
Lack of fetal heart activity can only be detected during an ultrasound examination and sometimes appears without additional symptoms. Unfortunately, it usually means a lack of fetal development.
Amniotic fluid is the natural living environment of the fetus. It is of great importance for its proper development and fulfills several necessary functions (among others, it protects and cushions, enables fetal movements, has a bactericidal effect, and supports lung development). The lack of amniotic fluid deprives the fetus of its most important protection.
Procedure
The appropriate method of therapy is contingent upon the patient’s clinical condition and the nature of the miscarriage. In cases of threatened miscarriage, it is advisable to recommend restricted activity, a conservative lifestyle, and the promotion of mental well-being for the patient. Conversely, in the case of a diagnosed aborted miscarriage, wherein the fetus has expired, pharmacological intervention is recommended. It entails the administration of prostaglandins to induce uterine contractions, facilitating the expulsion of the deceased fetus.

Uterine Curettage
It’s important to note the following information: if the use of prostaglandins fails to expel fetal remnants from the uterus completely, curettage of the uterine cavity becomes necessary. The need for curettage arises when there is 15mm thick material in the uterus, coupled with heavy uterine bleeding.
Material from a miscarriage should be submitted for histopathological examination, as this may facilitate the identification of the underlying cause of the miscarriage in some cases. It’s crucial to emphasize the significance of providing psychological support to women who have undergone a miscarriage.
Psychological Care After Miscarriage
We should not forget that miscarriage is an unpleasant experience for a large group of women and their partners. The mental aspect should always be taken into account in further proceedings. Patients should be provided with psychological support and, in justified cases, also psychopharmacological support. It can significantly reduce the psychological consequences of pregnancy loss, which can lead to depression and even suicide.
Another Pregnancy After A Miscarriage
The time it takes to get pregnant again after a miscarriage can vary depending on each woman’s individual health and emotional circumstances. You should consult a doctor who can assess your situation and advise you when would be the best time to get pregnant again.
Sources
- Early Pregnancy Loss (Spontaneous Abortion). NIH.
https://www.ncbi.nlm.nih.gov/books/NBK560521/ - Miscarriage. NHS.
https://www.nhs.uk/conditions/miscarriage/ - Symptoms. NHS.
https://www.nhs.uk/conditions/miscarriage/symptoms/ - Causes. NHS.
https://www.nhs.uk/conditions/miscarriage/causes/ - Evaluating the Clinical Risk Factors Associated With Miscarriages in Women in Karachi, Pakistan. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8610211/ - Signs and Symptoms of Early Pregnancy Loss. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5933199/ - Methods for managing miscarriage: a network meta‐analysis. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8168449/ - Dilation and Curettage. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK568791/ - Afterwards. NHS.
https://www.nhs.uk/conditions/miscarriage/afterwards/ - Trying to conceive after a pregnancy loss. NIH.
https://www.nih.gov/news-events/nih-research-matters/trying-conceive-after-pregnancy-loss