The disease may occur at any lactation stage but most often happens in the first weeks after delivery (2-6 weeks) and more often in the winter months. The inflammatory process may affect one or both breasts, but rarely, it affects both breasts at the same time.
Who else Can Get Mastitis?
Breast inflammation not related to lactation is much less joint. However, it is worth mentioning because, in addition to women, the disease can affect men, teenagers, and small children.
Postpartum mastitis (not related to breastfeeding or lactation) occurring in women reaches two peaks in incidence depending on age. Many cases occur in women under 30 years of age. The rest happen in women aged 50-60 years of age. The primary causes of postpartum mastitis include injuries, infection of the sebaceous and sweat glands, nipple piercing, implants, hyperprolactinemia, and thyroid dysfunction. Treatment involves administering anti-inflammatory drugs and antibiotics. If there is no improvement, further diagnostics are necessary to exclude cancer.
The action of maternal hormones causes enlargement of the mammary glands in newborns. Most cases do not require treatment and disappear within 2-3 weeks. Rarely, bacterial superinfection of the enlarged gland occurs, which leads to the development of neonatal mastitis requiring treatment.
In most cases, mastitis in men is caused by staphylococcal infection. Predisposing factors include hormonal disorders, alcohol abuse, use of anabolic steroids, and chest injuries. During therapy, pharmacological treatment is used.

Causes
Inflammation of the nipple (breast gland) is a condition that may affect many women, especially during the postpartum period. It is an inflammation that causes swelling, redness, and pain in the nipple. The causes of mastitis can differ, and it is significant to know them to avoid this unpleasant condition.
One of the primary causes of nipple inflammation is a bacterial infection. Bacteria such as Staphylococcus aureus, cutaneous bacteria, and streptococci can enter the nipple through broken skin or cracks in the nipple. It often happens during breastfeeding when the skin on the nipple becomes irritated.
Another factor contributing to mastitis is the baby not being properly attached to the breast. If your baby does not latch on to the nipple properly, it may lead to mechanical damage and irritation. Improper feeding techniques can also cause milk stagnation, which favors the development of infections.
Sometimes, nipple inflammation may be the result of an allergy or irritation. Agents such as chemical cleaning products, perfumes, creams, and soaps can cause allergic reactions or skin irritation. People with skin hypersensitivity may be more susceptible to this type of inflammation.
Other risk factors for nipple inflammation include:
- Incomplete emptying of the breasts
- Immune deficiencies that weaken the body’s immunity
- Previous breast inflammation
- Diabetes or other metabolic diseases
- Breast injury
- Chronic stress
- Smoking tobacco
- Improper nutrition
- Overproduction of milk caused by unnecessary pumping
To sum up, there are two ways of puerperal mastitis. The first one is called adenitis and occurs when the milk duct is blocked, or food stagnates, resulting in infection. The second one – cellulitis occurs through damaged breast skin, and the connective tissue of the breast gland becomes infected through the bloodstream.
It is also worth adding that non-puerperal mastitis is a rare phenomenon, occurring only in about 5% of all cases of mastitis. Non-puerperal mastitis can happen for various reasons. One of the most common is an inflammatory complication of mastopathic changes in the breasts. Other factors predisposing to the occurrence of the mentioned problem are:
- Hyperprolactinemia (disorder of pituitary gland function)
- Thyroid dysfunction
- Taking certain medications that lower blood pressure
- Nipple piercing or nipple injuries
- Breast enlargement using silicone implants
- Infection of the sebaceous and sweat glands
- Smoking
Additionally, sometimes the so-called cyst of Montgomery, is inflammation of one of the Montgomery glands on the nipple, leading to a boil and possibly an abscess.
It is worth noting that non-puerperal mastitis can occur in any woman, regardless of age or situation, although it more often affects women during the postpartum period.
Symptoms
Regardless of the type of mastitis, similar symptoms are noticed. The first signal worth paying attention to is pain in the nipple area. It may feel like a burning sensation, tension, or pulsation. The pain may also be accompanied by skin redness and swelling around the nipple.
Another characteristic symptom of mastitis is fever. In some cases, nipple inflammation can also cause an abscess to appear. It results from the accumulation of pus in the tissues, which causes a painful lump to form.
Along with the physical symptoms, nipple inflammation can also affect your overall well-being. You may feel tired, weak, and in a worse mood. If a woman experiences these symptoms along with pain in the nipple area, this is an additional signal that it may be mastitis.

Diagnosis
The diagnosis of mastitis is made by a doctor based on a physical examination and the observed symptoms of the disease (such as redness, warmth, swelling and pain of the breast or part of it, increased body temperature).
During the examination, the doctor must make sure that no breast abscess has developed, which (in addition to antibiotic therapy) also requires surgical treatment (biopsy or incision of the wall and emptying). Suppose the doctor cannot exclude the existence of an abscess based on a physical examination. In that case, they may perform an ultrasound examination of the breast (the image is obtained by applying an ultrasound-emitting transducer to the breast).
Rarely, when mastitis does not respond to standardly administered medications, the specialists perform the so-called “milk inoculation.” This diagnostic test aims to grow pathogenic bacteria from a food sample taken from the patient and determine what drugs they are sensitive to. To collect a sample, the woman should wash her breast, squeeze some milk out, and throw it away.
The next portion should be squeezed directly into a sterile container, avoiding contact of the container with the nipple. In the diagnostic laboratory, the contents of the container are “sown” into dishes filled with a particular substrate containing nutrients and then placed in incubators that maintain a constant temperature close to the human body temperature. In such conditions, microorganisms multiply rapidly, making recognizing them and determining drug sensitivity possible.
Sometimes it is necessary to perform a breast biopsy (taking a sample of its contents using a thin needle inserted under ultrasound guidance). This situation occurs in two cases:
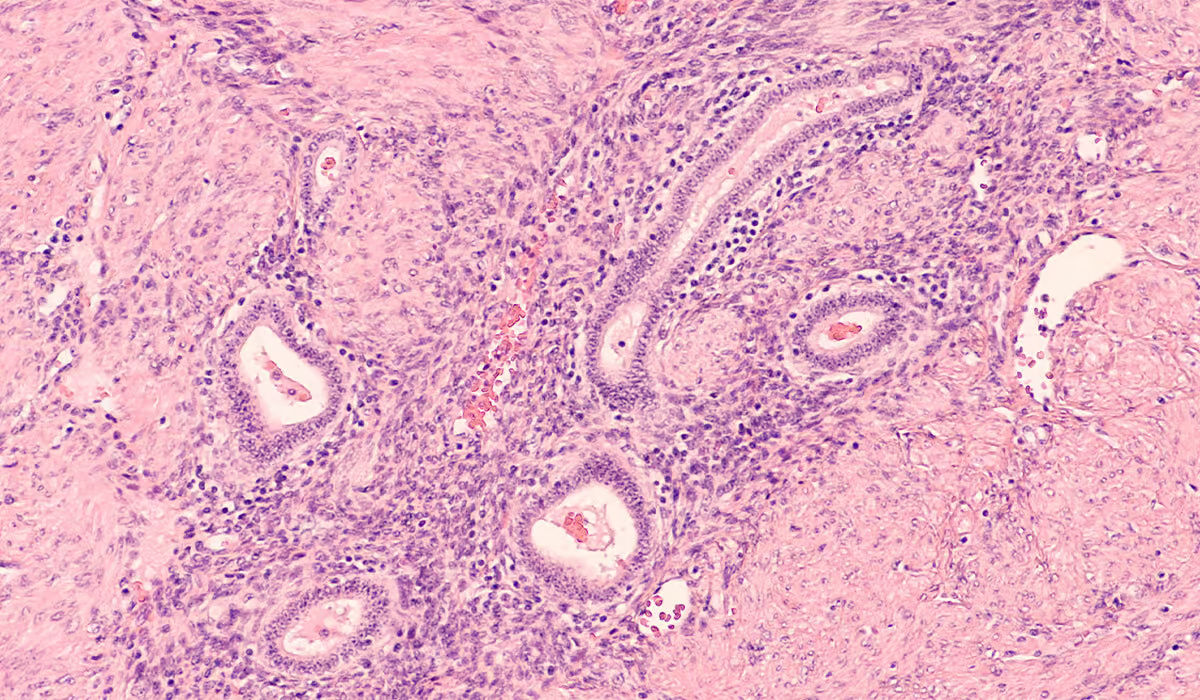
- The symptoms do not subside despite the implementation of appropriate antibiotic therapy – this may indicate the development of a rare type of breast cancer – the so-called inflammatory cancer, the symptoms of which (redness, swelling, and pain in the breast) are almost identical to those of mastitis. The biopsy sample is then subjected to cytological examination to determine or exclude the presence of cancer cells.
- An abscess has formed – the contents of the abscess collected by biopsy are used to perform a culture and determine the type of bacteria that caused the inflammation.
Treatment
The first step in treating non-puerperal mastitis is to consult a doctor. The specialist will be able to diagnose based on your symptoms and perform a physical examination. Additional diagnostic tests, such as a complete blood count, may also be necessary.
The main goal of treatment for non-puerperal mastitis is to fight the infection and alleviate the symptoms. In case of a bacterial infection, antibiotics may be necessary. Surgical intervention may be necessary if the inflammation progresses and an abscess forms. In such cases, your doctor may recommend drainage of the abscess to remove accumulated fluid and help the wound heal.
It is worth adding that the treatment of mastitis, both non-puerperal and puerperal, is similar. However, in the latter case, the woman is given non-steroidal anti-inflammatory drugs or additional drugs that will inhibit lactation.
Please remember that acute mastitis will not go away on its own. The best results are achieved by implementing a combined treatment, including antibiotic therapy prescribed by a doctor and “home” treatments:
- Antibiotic therapy – drugs should usually be taken for 10 to 14 days (it is significant that, despite the symptoms of the disease disappearing after a few days, the antibiotic treatment should be completed – thus minimizing the risk of disease recurrence)
- Using painkillers (e.g., paracetamol or ibuprofen to relieve the pain associated with inflammation)
- Rest and drinking plenty of fluids – allow the body to cope with fever and other symptoms of inflammation more quickly.
- Using creams with lanolin – brings relief to sore nipples
- Applying cold compresses to the breasts – using ice or gel compresses – reduces pain and swelling
- You cannot massage your breasts hard or force the milk out – such a procedure may lead to the extension of inflammation and the formation of a breast abscess.
- Frequent replacement of breast pads – so that they are clean and dry. If your nipples leak pus, they should be gently washed and dried before wearing a bra.
Regular emptying of healthy and diseased breasts is the most essential treatment method. It eliminates milk stasis, leading to further multiplication of bacteria and the development of inflammation. During acute mastitis and its treatment, you can and even must continue breastfeeding – milk from the affected breast is in no way harmful to the baby.

If possible, feed from the affected breast and provide it until it is empty (the breast will become soft). Sometimes the baby has problems with correctly grasping and sucking the inflamed breast. It is usually caused by the breast being too hard – it is worth trying to express some milk from it before starting to feed, making it easier for the baby to grasp it.
Most women can breastfeed throughout the inflammation and its treatment. However, if the pain during feeding is too severe and the woman gives up feeding the affected breast, remember to regularly express milk from that breast using her hands or a breast pump.
Treatment of Abscess
Treatment for a breast abscess includes:
- Surgical incision of the abscess under local anesthesia and emptying its cavity
- Insertion of drainage – a small tube or tubes that drain the remaining pus (they are removed after about 5-7 days)
- Antibiotic therapy – oral or (rarely, when the disease is advanced) intravenously
- Regular emptying of the breasts (through breastfeeding, using your hands, or a breast pump)
If your doctor orders you to stop breastfeeding the affected breast until the abscess heals, remember to express milk regularly using your hands or a breast pump. Breastfeeding a healthy breast while treating an abscess is safe for the mother and baby.
Antibiotic Therapy and Breastfeeding
Breastfeeding during antibiotic therapy to treat mastitis is entirely safe for the baby. Many antibiotics differ in their method and scope of action – they are effective against a specific group or groups of pathogenic bacteria. Antibiotics prescribed by a doctor and used during breastfeeding do not harm the baby (which has been proven in studies) – provided they are used according to medical recommendations.
Taking small doses of painkillers for a short period (sufficient to control the symptoms of mastitis) is also safe for a breastfed baby.
During pregnancy and breastfeeding, use only medications recommended by your doctor and never change the doses recommended by your doctor (do not increase or decrease them) – this way, you will be sure that your child is safe.
What Should Breast Care Look Like During Pregnancy and Lactation?
The period of pregnancy and breastfeeding is a demanding time for a woman’s breasts. Changes related to breast enlargement may cause itching and lead to stretch marks. Regularly moisturizing your breasts should provide relief, both during pregnancy and lactation.
Typically, breasts enlarge most on the third day after giving birth, when the milk supply begins. During this time, you should pay special attention to what you use to care for them. Remembering that your baby’s face will be touching the breast, it is best to choose moisturizing products for newborns.
During milk production, you should not perform massages because the breasts are very delicate, and the structures inside are swollen and heavily overloaded. Massage may damage the ducts, leading to inflammation of the breast and, in extreme cases, to the formation of an abscess.
During pregnancy and breastfeeding, we must not forget about the prevention of breast diseases. There are no contraindications to resigning from regular ultrasound examinations. Self-examination is also very important, although breastfeeding may make it more difficult to perform accurately. It happens because milk-filled structures can distort the image during palpation. It is worth remembering that breasts are changing dynamically during this period – something that will be normal in the 5th week of lactation may mean pathology in the 25th week of lactation. For your own peace of mind, if you are concerned about something, it is best to consult a doctor.
Sources
- Postpartum mastitis in the breastfeeding women and antimicrobial resistance of responsible pathogens in ukraine: results a multicenter study. NIH. https://pubmed.ncbi.nlm.nih.gov/32386365/.
- Granulomatous mastitis in a male breast: A case report and review of literature. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9981576/.
- Mastitis and Breast Abscess in Newborns and Infants. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9615954/.
- Incidence of and Risk Factors for Lactational Mastitis: A Systematic Review. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7672676/.
- Acute Mastitis. NIH. https://pubmed.ncbi.nlm.nih.gov/32491714/.
- Mastitis. NHS. https://www.nhs.uk/start-for-life/baby/feeding-your-baby/breastfeeding/breastfeeding-challenges/mastitis/#causes-of-mastitis.
- Cyst of Montgomery: An uncommon adolescent breast lump. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7415277/.
- Mastitis. NHS. https://www.nhs.uk/conditions/mastitis/.
- Breast Infection: A Review of Diagnosis and Management Practices. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6092150/.
- Granulomatous mastitis diagnosed by core-needle biopsy and successfully treated with corticosteroid therapy: a case report. NIH. https://pubmed.ncbi.nlm.nih.gov/14634520/.
- Breast abscess. NHS. https://www.nhs.uk/conditions/breast-abscess/.