How Can You Get Infected With Leptospirosis?
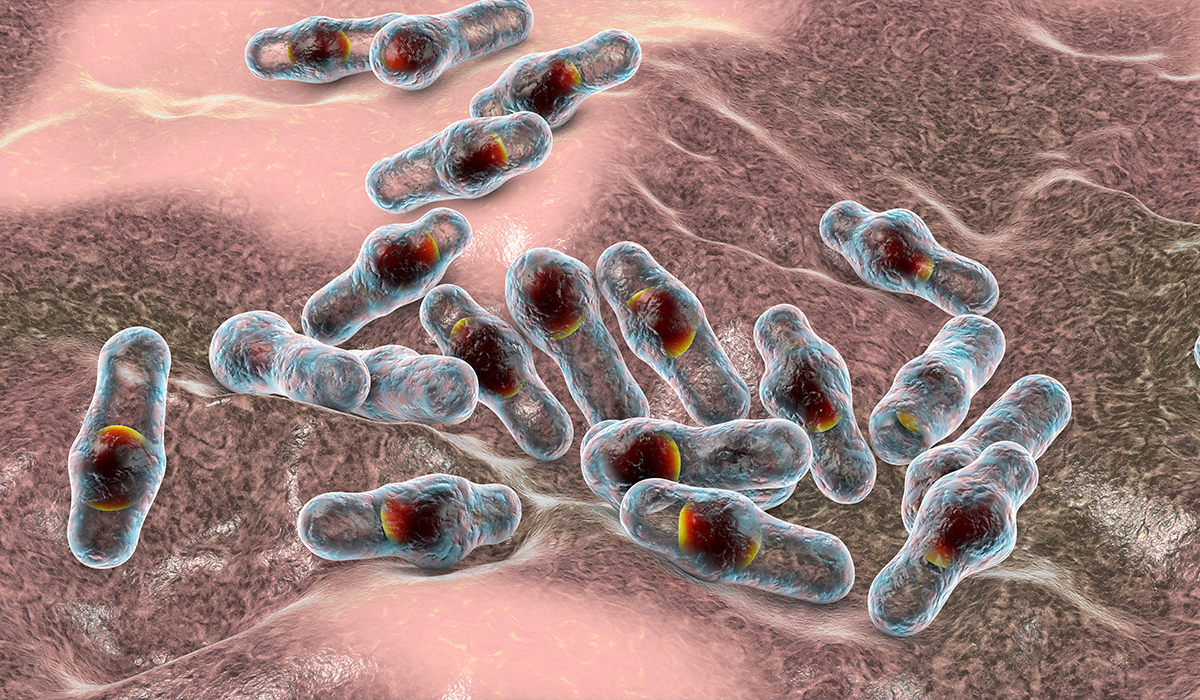
Leptospirosis spirochetes are bacteria that are most often transmitted by rats or other rodents but can also occur in many other animals: mammals, birds, and amphibians.
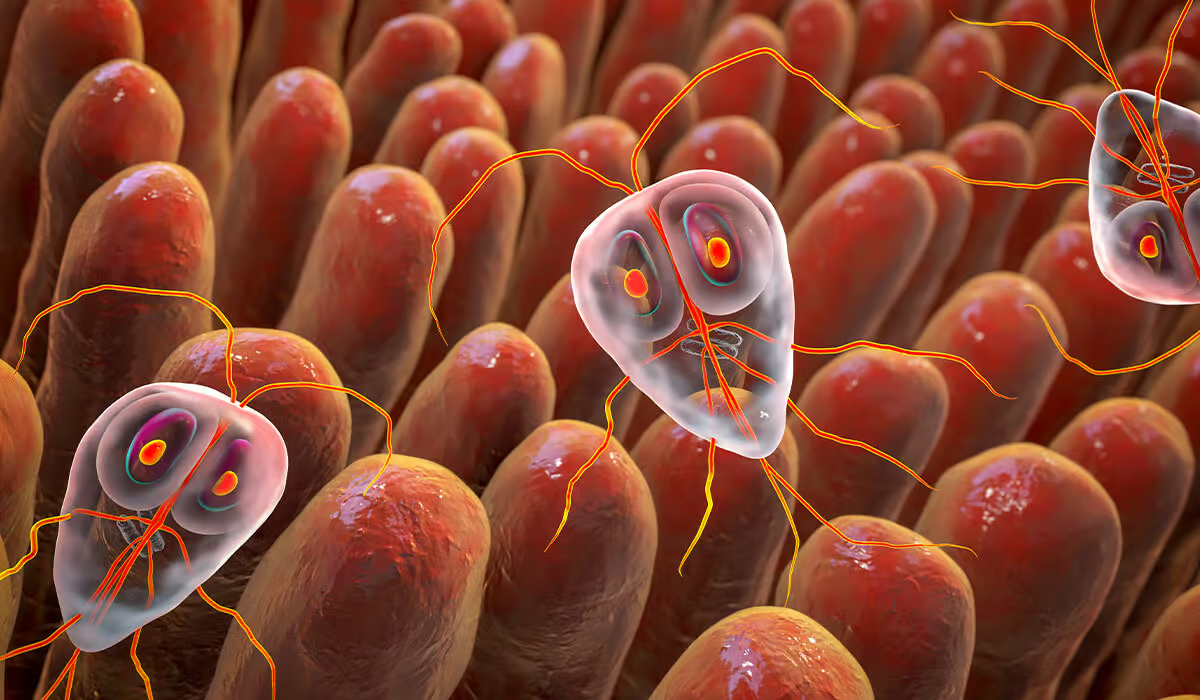
Infection with Leptospira spirochetes usually occurs through accidental contact with a sick rodent’s body fluids, mainly urine. The bacteria persist in contaminated soil and water, through which they are often transmitted. Spirochetes penetrate the body through mucous membranes, damaged skin, conjunctiva, and the digestive and respiratory systems. Sometimes, this condition occurs after being bitten by a sick animal or person, through blood, after sexual intercourse, and through the placenta during pregnancy.

Phases
We divide two leptospirosis phases: the leptospiremic (acute) and immune (delayed). The individual usually experiences mild symptoms or no signs in the first stage. Some individuals develop severe signs in the latter phase.
Leptospiremic Phase
In the leptospirosis phase (acute phase), the individual can experience a sudden onset of flu-like symptoms. It usually begins within 2 to 14 days after getting infected. This stage may last between 3 and 10 days.
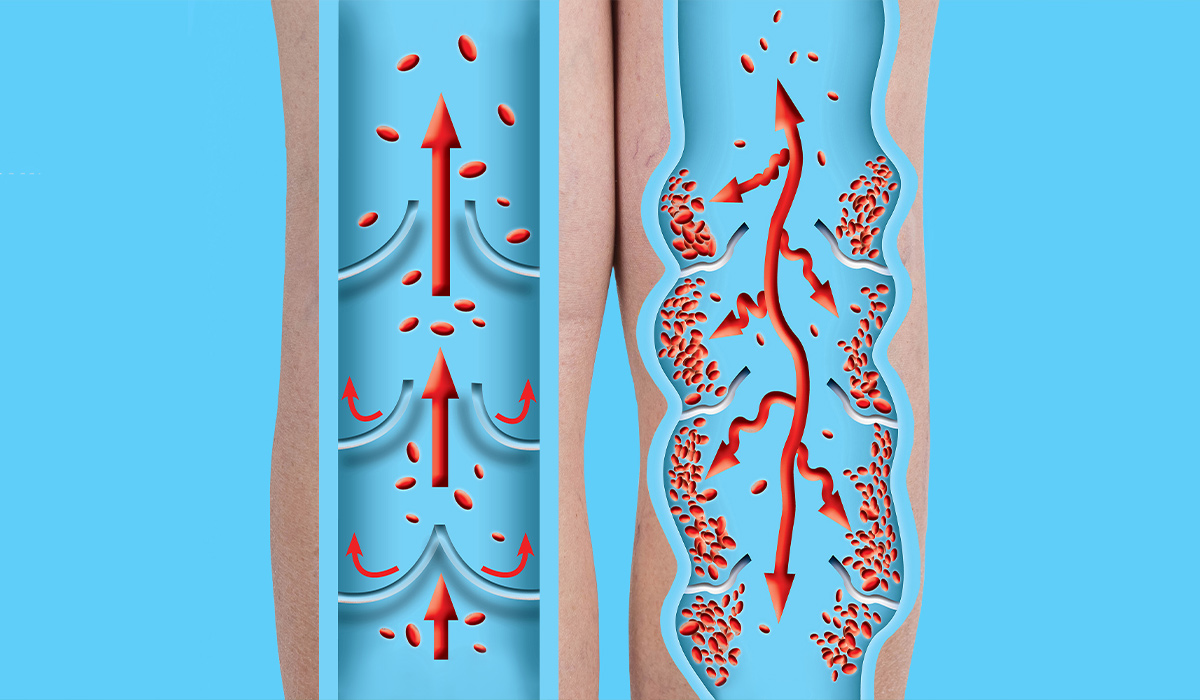
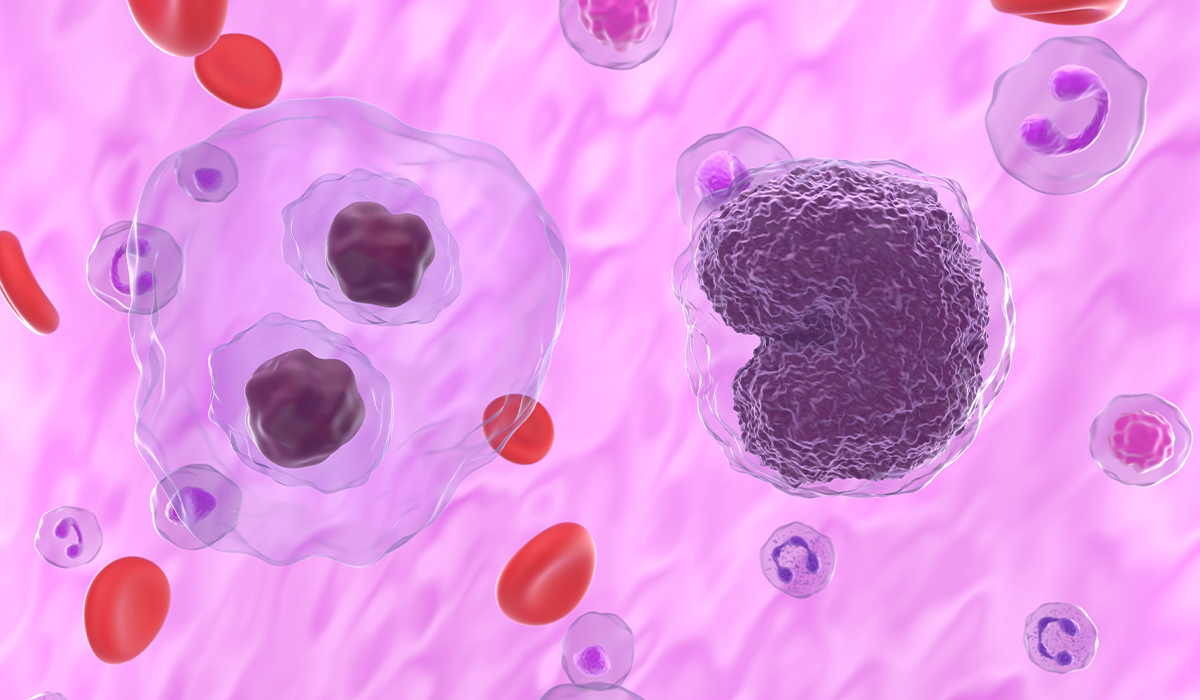
During this phase, Leptospira bacteria are in the blood. Those microorganisms move to the organs and may cause further health problems. Fortunately, blood tests will reveal indications of infection and make treatment possible.
Immune Phase
In the second stage (immune phase), bacteria have moved from the bloodstream to the organs. It mostly concerns the kidneys. That is why urine tests will reveal signs of the bacteria’s presence. There will also be antibodies to Leptospira in the blood.
Some individuals will get ill with Weil’s disease during this stage. It induces internal bleeding, kidney damage, and severe yellowing of the skin and eyes (jaundice).
Causes
The typical cause of leptospirosis is a bacteria called Leptospira interrogans. Many animals carry it, and it lives in their kidneys – then contacts soil and water from their urine.
If the individual is near soil or water where an infected animal has peed, the germ can invade the body through breaks in the skin. It happens especially when scratches, open wounds, or dry areas occur. It may also get to the organism through the nose, mouth, or genitals. It is challenging to get it from another individual, however – it may be transmitted during sexual intercourse or breastfeeding.
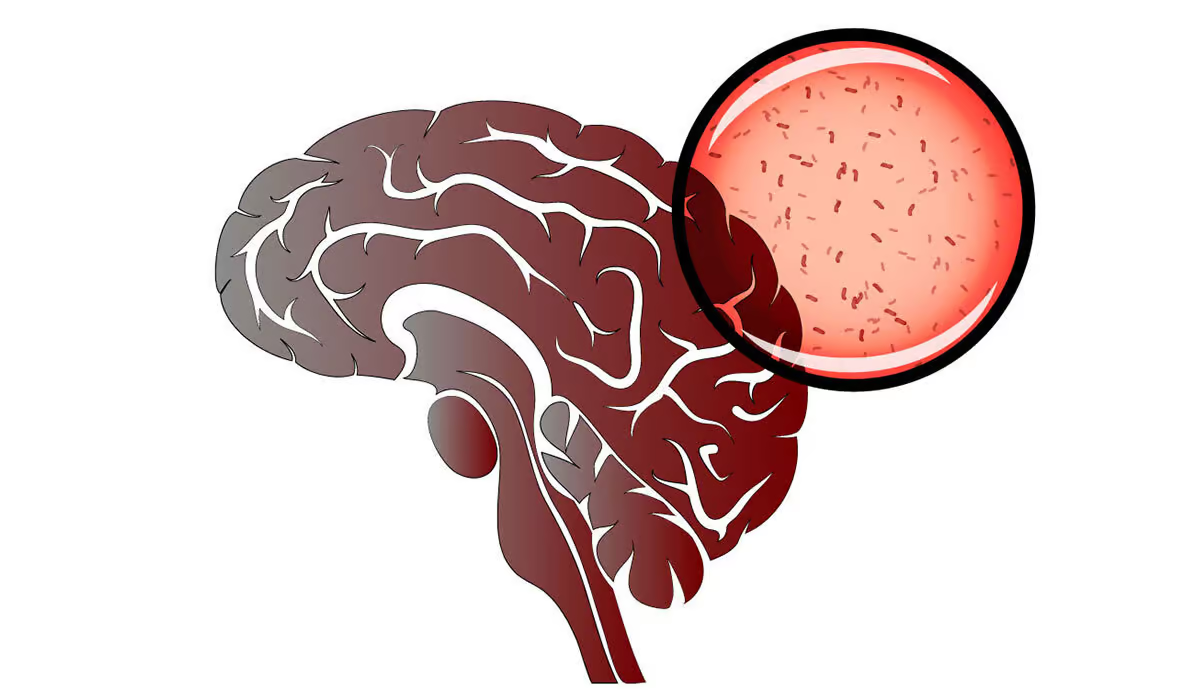
After entering the body, Leptospira spirochetes spread through the blood. This way, they reach the organs of almost all systems. Bacteria can cross barriers that protect significant organs, such as the brain and eyeball. Additionally, Leptospira spirochetes can damage small blood vessels and lead to their inflammation and organ changes. Typically, bacteria begin to multiply in tissues about two weeks after infection, which is associated with the appearance of symptoms.
Who Is At Risk?
Leptospirosis is more likely to impact individuals who:
- Live in tropical or temperate climates
- Work with animals (e.g., dairy farmers or veterinarians)
- Work outdoors (e.g., mine or sewer workers)
- Camp outside
- Participate in outdoor sports
- Live in areas with flooding or improper sanitation
- Garden or handle potentially contaminated soil
Specificity of Leptospira Infections
Leptospirosis is most common in tropical climate zones.
Animals are the reservoir of infection, and the environment plays an increasingly smaller role in the survival of leptospires. In temperate climate zones, an increase in the number of infections spread through the environment, mainly through water contaminated with leptospires, is observed in the summer months and early autumn. A more frequent occurrence of leptospira infections is observed in countries and regions with larger natural water reservoirs, wetlands, or, for example, a more developed network of canals than in areas with less water resources.
Additional factors contributing to the spread of leptospira infections in temperate climate zones are the climate changes observed in recent decades and the increasing population movement. In European countries and North America, cases of leptospirosis are increasingly reported among people who became infected during tourist trips to tropical countries. It is facilitated by, among others, the growing popularity of active forms of recreation.
Symptoms
Symptoms of leptospirosis vary depending on the stage of the disease. The first one is related to bacteremia, i.e., the spread of spirochetes into the blood. The condition has a sudden beginning, and the first symptoms of leptospirosis resemble a cold.
Patients complain of headaches, general weakness, chills, cough, fever (approximately 39-40 degrees Celsius), muscle pain, sore throat, and loss of appetite. Additionally, nausea, vomiting, conjunctivitis, photosensitivity, joint pain, and skin rash may occur.
The first phase of the condition usually lasts about seven days. In most patients, the course of leptospirosis is mild. After a week, the symptoms usually disappear on their own. Patients stop having fevers and feel better.

The second period of the disease is related to the body’s immune system response. Patients complain of very severe headaches, neck stiffness, and photophobia, which are symptoms of meningitis. The high fever returns, accompanied by shortness of breath, abdominal pain, reddened conjunctiva, and even hemoptysis.
In some cases, jaundice appears. Severe icteric leptospirosis is called Weil’s disease. Additionally, kidney damage occurs, manifested by hematuria and proteinuria. Hemorrhagic skin lesions, nosebleeds, and hemoptysis may also occur.
Diagnosis
If you experience symptoms of leptospirosis, be sure to see a doctor. In mild cases of the disease, treatment is not necessary, and the symptoms tend to be self-limiting.
The first stage of the disease is often not correctly recognized due to non-specific, flu-like symptoms. Symptoms that suggest urgent further diagnostics include poor health, severe shortness of breath, hemoptysis, jaundice, hematuria, and oliguria (i.e., urination in small amounts).
An interview helps diagnose the disease. Infections with Leptospira spirochetes are suggested by, e.g., working in professions particularly exposed to infections, recent trips to tropical countries, swimming in ponds and lakes, practicing water sports, and frequent contact with animals.
Diagnostics is based on the isolation of Leptospira from internal organs (liver, lungs, brain, and kidneys), body fluids (blood, milk, cerebrospinal, pleural, and peritoneal fluids), demonstration of the presence of the germ or its nucleic acid in tissues and body fluids, and on results of serological tests aimed at detecting antibodies specific to this germ.
Analysis of the epizootiological situation raises the suspicion of leptospirosis, and clinical and autopsy examinations are helpful in the correct diagnosis of the disease. However, the clinical and autopsy examination itself has limited diagnostic value. Isolation of the germ is challenging and requires several weeks. Serological tests, especially the microscopic agglutination test (MAT) and ELISA, are of decisive importance in the diagnosis. To identify leptospires, an immunohistochemical test and PCR are recommended.
Treatment
The treatment consists of using antibiotics. However, in mild cases, the specialist can have the patient keep an eye on their symptoms to notice if the infection gets better without any treatment.
In the case of severe leptospirosis, a stay in the hospital is helpful. The health provider can give the medication straight through a needle connected to a tube that brings medicine to your blood (an IV). Depending on which organs are affected, you can require additional medications or procedures.
Leptospirosis is treated with antibiotics. The choice of antibiotic depends on the medical history and the severity of the illness, which the healthcare provider will determine.

Supporting Treatment
The patient can have breathing troubles if the lungs are contaminated with bacteria. In this case, they may need the help of a machine to breathe for them.
Plasmapheresis might help if the patient is at risk for organ damage from leptospirosis. This process allows the specialist to remove the blood using a tube connected to a vein. A machine divides the plasma from blood and replaces it with a plasma substitute. Then, it returns to the organism through another pipe.
Patients with a complicated form of the disease usually require treatment to support the function of significant organs. It mainly includes supporting the functioning of the liver and kidneys. Additionally, there may be a need to treat neurological and cardiovascular complications and hemorrhages.
Complications
Treatment may help ease the severity of this condition. However, without therapy, it can end in developing complications. Those include:
- Meningitis
- Liver failure
- Kidney damage (which may lead to kidney failure)
- Respiratory issues
- Hemodynamic collapse
- Death of a fetus (in people who are pregnant)
- Death
Prevention
To minimize the risk of infection with this potentially dangerous disease, you should follow basic hygiene rules, i.e., wash your hands before each meal and after playing with animals.
Combating rodents as the carriers of Leptospira spirochetes, including residential buildings and farm rooms where pigs, cattle, goats, sheep, and other farm animals are kept.
Use protective clothing, rubber gloves, and rubber shoes when working with animals. Do it, especially if there are abrasions or wounds on the skin.
Avoid consumption of raw water and unwashed vegetables and fruits from places where there is a risk of environmental contamination with bacteria excreted in the urine of infected wild and farm animals.
Veterinary service workers should use protective masks to protect against the inhalation of potentially infected bioaerosol, especially in breeding rooms (piggeries and barns).
Perform initial, periodic, and ongoing diagnostic tests for veterinary service employees.
Vaccines used in humans to a limited extent help protect groups of people living in tropical zones who are most at risk of infection. However, the immunity they induce is still not satisfactory and work is still ongoing to improve them. Vaccines used in animals allow for obtaining relatively short-term immunity only to antigens of serotypes or serogroups contained in a given biopreparation.
Administration of antibiotics to people and animals in various programs is also quite effective, although burdened with significant drawbacks, in preventing infections. However, apart from other imperfections, this action is quite expensive due to the need for systematic and long-term administration of chemotherapy drugs.
Prevention While Your Pet Has Leptospirosis
If your pet is infected with leptospirosis, here is what you can do to protect yourself:
- Give the pet the prescription antibiotics, as ordered by the specialist
- Avoid interacting with pet’s urine
- If the pet pees in the house, clean it instantly
- Wash your hands after touching your pet
Prevention In Dogs
The course and symptoms of leptospirosis in dogs vary depending on the serovar and sometimes the strain of Leptospira, the age of the dogs, their immune status, and their gender.
Sometimes leptospirosis is asymptomatic in some dogs, mild in others, and in some dogs, its course is severe and ends in death. Clinical symptoms are diverse, and none are pathognomonic. The disease usually begins with fever, chills, depression, loss of appetite, muscle pain, weakness, and stiff gait. Often the mucous membranes are congested.
Over time, signs of renal involvement may appear, as evidenced by anuria or frequent urination, hematuria, vomiting, dehydration, and oral ulceration. Miscarriages, diarrhea, jaundice, cough, shortness of breath, and conjunctivitis may also occur. Some dogs have a hemorrhagic syndrome characterized by petechiae and hemorrhages on the mucous membranes. Later in the syndrome, hemorrhagic inflammation of the gastrointestinal tract develops, and bleeding from the nostrils also occurs. Kidney involvement is common.
The only way to see if your pet has leptospirosis is to ask your vet for a test.
Vaccines based on recombinant Leptospira membrane protein, lipopolysaccharide vaccines, inactivated and attenuated vaccines, and DNA vaccines are increasingly recommended among the newly developed vaccines. Vaccination significantly reduces the percentage of animals infected with existing exposure and protects against abortions.
Post-vaccination immunity lasts from 6 months to a year. The essential condition for vaccine effectiveness is the presence of antigens in the vaccine for the leptospira serotypes that cause infection. Otherwise, vaccinations will not bring the intended effect. However, vaccination does not prevent the carrier from shedding the disease in urine.
Sources
- Pathogenesis insights from an ancient and ubiquitous spirochete. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8530280/ - Leptospirosis. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK441858/ - Leptospirosis: clinical aspects. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8813018/ - Fulminant Leptospirosis (Weil’s disease) in an urban setting as an overlooked cause of multiorgan failure: a case report. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3025967/ - Leptospira. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK8451/ - Studying Risk Factors Associated with Human Leptospirosis. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3982353/ - Environmental and Occupational Factors Associated with Leptospirosis: A Systematic Review. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10761560/ - Leptospirosis Diagnosis: Competancy of Various Laboratory Tests. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3939550/ - Two Methods for Rapid Serological Diagnosis of Acute Leptospirosis. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC96061/ - Immunohistochemical detection of Lp25 and LipL32 proteins in skeletal and cardiac muscles of fatal human leptospirosis. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7653813/ - Diagnosis of human leptospirosis: systematic review and meta-analysis of the diagnostic accuracy of the Leptospira microscopic agglutination test, PCR targeting Lfb1, and IgM ELISA to Leptospira fainei serovar Hurstbridge. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10848445/ - Antibiotics for the Treatment of Leptospirosis: Systematic Review and Meta-Analysis of Controlled Trials. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3733179/ - Role of Plasmapheresis and Extracorporeal Membrane Oxygenation in the Treatment of Leptospirosis Complicated with Pulmonary Hemorrhages. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6304550/ - Leptospirosis and its complications. NIH.
https://pubmed.ncbi.nlm.nih.gov/22312885/ - Prevention and treatment of leptospirosis. NIH.
https://pubmed.ncbi.nlm.nih.gov/15482194/ - Leptospirosis vaccines. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2231387/ - Potential Drivers for the Re-Emergence of Canine Leptospirosis in the United States and Canada. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9694660/