Chilling leads to a slowdown in metabolic processes and, above all, to disturbances in consciousness and reduced efficiency of the body’s work, which may be a direct cause of an accident.
Paramedics and doctors rarely measure temperature with a thermometer to diagnose hypothermia. Assessment is usually made by observing general symptoms and body reactions.

Is Lowered Temperature Dangerous?
The standard body temperature of a healthy adult is between 36.6 and 37 degrees Celsius. A reduced temperature is below 36.6 but above 35 degrees. Even lower values are called hypothermia, i.e., cooling of the body.
A slightly lowered temperature does not threaten health or life, but it may be a symptom of many serious diseases, especially if it persists for a long time. Before concluding, however, you should check the readings’ accuracy using another thermometer (electronic devices tend to underestimate the results).
The place of measurement (under the arm) and its technique (the thermometer should be pressed well against the body) are also important. It is also worth measuring the temperature at different times of the day, remembering that in the morning, it is usually lower than in the evening, even by 0.5 degrees Celsius.
Causes
There can be many causes of body hypothermia. In older people, physiological thermoregulation mechanisms often function incorrectly. In turn, children freeze faster due to an unfavorable ratio of body weight to its surface area and the inability to assess the situation (e.g., playing in the water for a long time despite feeling cold).
Hypothermia is also promoted by alcohol consumption, which causes blood vessels to relax and increase heat loss, as well as reducing muscle tremors. Some psychoactive substances may have a similar effect.
Selected diseases increase the risk of hypothermia:
- Metabolic (e.g., diabetes and its complications or including damage to blood vessels)
- Neurodegenerative (e.g., Parkinson’s disease or multiple sclerosis)
- Hormonal causes (hypothyroidism, pituitary or adrenal gland insufficiency)
They all influence not only the body’s thermoregulation but also the subjective feeling of cold.
Factors increasing the risk of hypothermia include:
- Old age – elderly individuals have impaired thermoregulation and additional comorbidities.
- Babies and children – infants do not have sufficiently efficient mechanisms for regulating heat production. Children have a large ratio of the surface area through which they lose heat compared to their body weight. That is why the heat loss is more significant. Moreover, if left unattended, they cannot predict the consequences of staying in an environment that is too cold (e.g., bathing in an open tank or playing in the snow).
- Mental disorders – people with incorrect assessment of the environment and memory problems are exposed to long-term stay in a cold environment because they cannot assess the risk associated with it.
- Alcohol and drug abuse – the influence of intoxicants can predispose to hypothermia in several ways—disturbed orientation and assessment of the situation, clothing inappropriate to external conditions. Frequent cases of falling asleep under the influence of alcohol or falling into water extend the time of exposure to cold. Thermoregulation disturbed by alcohol causes dilation of blood vessels in the skin and thus increases heat loss, and the natural defense reaction to cold, i.e., muscle tremors, is also weakened.
- Concomitant diseases – some metabolic and hormonal disorders may cause insufficient thermoregulation, e.g., hypothyroidism, malnutrition, anorexia, diabetes (which causes sensory disturbances in the limbs due to diabetic neuropathy), and dehydration. Neurological diseases, e.g., Parkinson’s disease, previous stroke, and spinal cord damage, impair the perception of cold.
- Medicines – sedatives, antidepressants, and narcotic analgesics may change the feeling of cold and thermoregulation.
Symptoms
In the first stage of hypothermia, when the body temperature reaches 32-35 degrees Celsius, the person is conscious but shivers. The body, feeling that it is losing the temperature necessary for the proper functioning of all organs, tries to raise it by forcing the muscles to move.
Shivering is the first sign that you must look for a place to warm up or put on layers of clothing to retain heat. In the shivering stage, there is slight cooling – just getting to a warm place, drying yourself if your body is wet, and drinking hot fluids to warm up can help.
When chills and cold hands and feet are accompanied by other symptoms, e.g.:
- Muscle tremors
- Weakness
- Dizziness
- Confusion
Then, you are dealing with mild hypothermia. At this stage, a person still can act on their own – to get to a place where help will be provided, to light a fire, or to make other attempts to warm themself.
In the second stage of hypothermia, when the temperature is from 28 to 32 degrees Celsius, there are no more chills. Still, the level of consciousness is lowered, speech and motor coordination are impaired – muscles are stiff, movements are incoherent, speech is slurred, the person is apathetic and loses track of time. In this condition, they require help from others.
In the third stage of hypothermia, when the body temperature is 24-28 degrees Celsius, the person loses consciousness and looks as if dead – the skin is blue-green, the pulse and breathing are barely felt or symptoms of respiratory and circulatory arrest, the pupils do not react to light. At this stage, resuscitation is necessary.
In the fourth stage of hypothermia, circulatory arrest occurs when the temperature drops below 24 degrees Celsius. Stage five is irreversible hypothermia, i.e., death.
Treatment
Although the pathophysiology and clinical discoveries of this condition appear along a continuum, the commonly accepted definition separates hypothermia into three types: mild, moderate, and severe. It is significant to use during diagnosis special low-reading thermometers because standard ones measure only as low as 34.4 degrees Celcius. Core temperature measurement is necessary to diagnose and control hypothermia. The gold standard is measurement in the lower part of the esophagus, but this is only possible in unconscious and intubated patients. An alternative is to measure the temperature in the rectum. However, temperature monitoring in this way may be distorted when the bladder is flushed with warm fluids or when the rectum is filled with large amounts of feces.

Due to its convenience, temperature measurement from the tympanic membrane may be an appropriate initial tool for pre-hospital use. Still, the hospital should replace it with a more accurate method. It is essential that the thermometer used can accurately measure a wide range of temperatures. The most straightforward thermometers from the pharmacy have a lower measurement limit of 34 degrees Celsius. We need a thermometer whose range of possibilities starts from 10 degrees Celsius.
We must treat a hypothermic person should very carefully. In case of mild symptoms of hypothermia, when the injured person is fully conscious, they should be undressed from wet clothes and, if necessary, cut their clothes.
It is also important to isolate the injured person from the cold. A conscious person can be given sweet, warm drinks, but a chilled person should not be given alcohol. Unconscious people with hypothermia must not be given any drinks, transport in a vertical position and undressing should be avoided, and medical assistance should be provided as soon as possible.
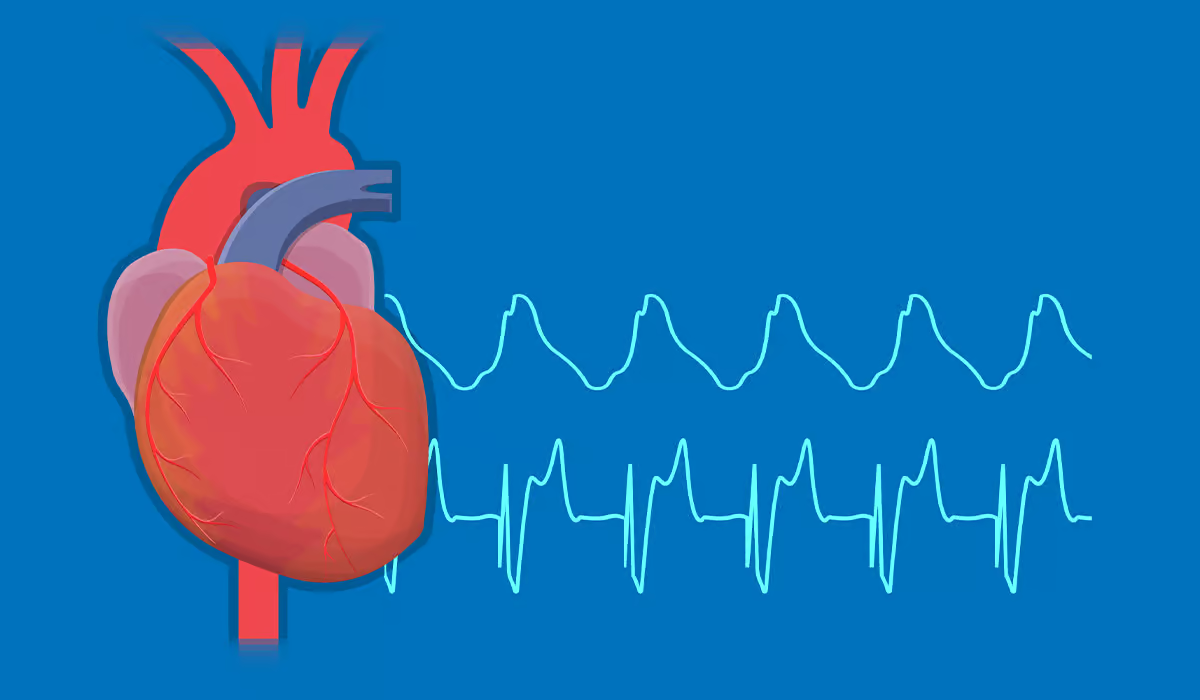
A victim of hypothermia in a state of deep hypothermia is often challenging to distinguish from a deceased person. The first aider should carefully assess the presence of a preserved circulation to avoid resuscitating a patient who has a preserved circulation. In this case, resuscitation undertaken too early may lead to disruption of the slow heart rhythm, trigger ventricular fibrillation, and worsen the patient’s condition.
Emergency teams may use a heart monitor with an ECG recording or an ultrasound scanner to assess the heart rhythm of a hypothermic person. That is because initially when hypothermia is mild, we may observe sinus tachycardia. Deepening hypothermia leads to further disorders. We can observe changes in the rhythm – atrial fibrillation is expected, followed by bradycardia, up to ventricular fibrillation and urokolia. Conditions such as atrial fibrillation do not need specific treatment and usually disappear with warming.
Advanced hypothermia always requires hospitalization. The doctor will assess the patient’s health in terms of hypothermia and the occurrence of possible frostbite. There are four categories of frostbite. Their treatment primarily involves gradually raising body temperature. Moreover, specialists try pharmacologically increasing peripheral circulation and elevating the limb to reduce swelling. If necrotic changes occur, the damaged tissues are removed.
The first step is to stop heat loss. We lose heat through:
- Evaporation of water from the skin’s surface
- Convection – heating of the air with which the body is in contact
- Heat radiation to the outside
- Conduction – transfer of heat directly to the environment (dominant in the case of immersion in water)
We lose most of the heat through the skin. Therefore, the most important thing is that we secure this road. Potential chilled patients should be placed in a warm and dry room. Specialists remove the patient’s wet clothes. Importantly, they undress the patient only when they are already in the room (at least in the ambulance). Please do not take off our clothes outside in the open. Cover dry skin with dry blankets; sleeping bags work great. NRC metalized foil has poor thermal properties and can be used as an addition; it cannot constitute the primary insulating layer.

At this stage, it should be emphasized how important it is to protect the patient against hypothermia during medical activities. Specialists usually prefer the patients to be undressed and exposed – because then they can do an EKG, insert an intravenous line, or connect a monitor. Unfortunately, this can lead to hypothermia even in patients who were not initially hypothermic.
Remember that hypothermia does not only happen in winter. Although looking for hypothermia in the warm months is unintuitive and easy to forget about it, it can also happen in summer.
Complications
One of the consequences of hypothermia may also be frostbite. It mainly affects the areas of the body with the least blood supply, i.e., fingers and nose.
A separate problem resulting from cold (temperature above 0°C) and moisture is tissue damage. Freezing does not occur in the limb, but as a result of long-lasting hypothermia and often too tight footwear, the vessels become constricted, and the chronically ischemic skin is irreversibly damaged. The foot is swollen, blue, and cold. The depth of damage to frostbitten layers is divided according to a four-point scale.
First-degree frostbite affects the superficial layer of the skin. It is waxy pale, and sensory disturbances, such as hyperesthesia, i.e., excessive sensitivity to touch and pain, may occur. Second-degree frostbite is characterized by the formation of blisters on the second or third day after the injury, and there is no pain sensation. Third-degree frostbite is much deeper and affects the skin throughout its entire depth.
The skin is warm. A fluid-filled blister can occur after rewarming the skin. If you have fourth-degree frostbite, your skin turns black because your cells die after freezing. On your skin, a hard, black covering might develop – it will fall off on its own. If it doesn’t, a specialist will remove it during surgery.
Sources
- Temperature. NIH. https://www.ncbi.nlm.nih.gov/books/NBK331/.
- Hypothermia. NIH. https://www.ncbi.nlm.nih.gov/books/NBK545239/.
- Incidences of underlying causes of hypothermia in older patients in the emergency department: a systematic review. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10261225/.
- Hypothermia. NHS. https://www.nhs.uk/conditions/hypothermia/.
- Hypothermia: risk factors and guidelines for nursing care. NIH. https://pubmed.ncbi.nlm.nih.gov/14705345/.
- The Hazards of Hypothermia. NIH. https://newsinhealth.nih.gov/2023/12/hazards-hypothermia.
- An evaluation of the Swiss staging model for hypothermia using case reports from the literature. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4756507/.
- Diagnosis and treatment of hypothermia. NIH. https://pubmed.ncbi.nlm.nih.gov/15617296/.
- Emergency treatment of hypothermia. NIH. https://pubmed.ncbi.nlm.nih.gov/11476420/.
- Hypothermia and cardiac electrophysiology: a systematic review of clinical and experimental data. NIH. https://pubmed.ncbi.nlm.nih.gov/30544147/.
- Accidental Hypothermia: 2021 Update. NIH. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8744717/.
- Frostbite. NIH. https://www.ncbi.nlm.nih.gov/books/NBK536914/.