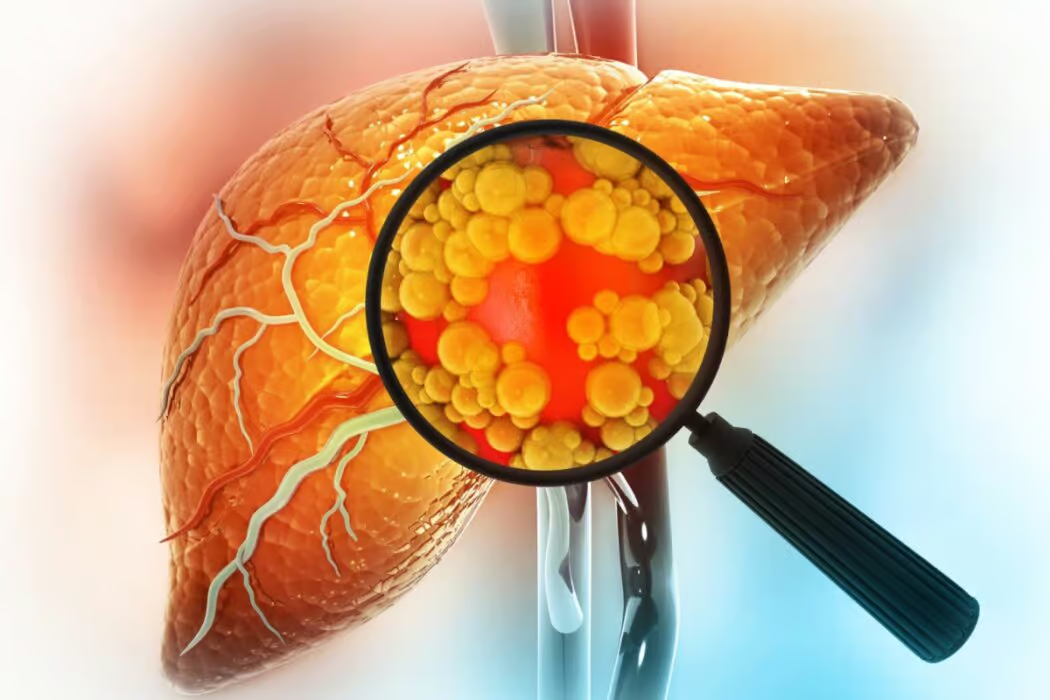
The action of a toxic substance may cause fatty liver disease – often alcohol, and it is then called alcoholic fatty liver disease, or if there is no specific cause, then it is called nonalcoholic fatty liver disease.
Fatty liver disease is otherwise called steatosis. A normal liver contains very little fat. The doctors diagnose steatosis if the fat content in the liver exceeds 5% of its weight.
What Functions Does The Liver Perform in Your Body?
The liver is one of the heavier organs of our body – it weighs 1.5 kilograms and is located on the upper right side of the abdomen. The liver consists of the right, left, quadrate, and caudate lobes, which are composed of hepatocytes – liver cells. Blood flows to the liver from two different sources:
- hepatic artery (which accounts for 20-30% of the blood supply)
- portal vein (70-80% of the blood supply)
and flows out through the hepatic vein.
The portal vein supplies blood from various organs, including the intestines and pancreas, and that is why excess nutrients flowing from the digestive system, e.g., glucose, are stored in the liver.
The liver is a vital organ – it performs over 500 different bodily functions. The most important of them include:
- Detoxification – The liver is the primary source of removal of toxins from the entire body
- Protein production – The liver produces around 85% of plasma proteins, which include proteins essential for blood clotting and albumins.
- Cholesterol production
- Glucose metabolism and storage – If there is an excess amount of glucose in the blood, the liver converts it into glycogen and stores it. Then, when the body needs glucose, glycogen can be broken down into glucose again and used by the body.
- Vitamin storage – the liver acts as a storage of vitamins, such as vitamins A, D, and B12.
- Bile production – The liver secretes bile to digest fat and absorb many health-important vitamins in the small intestine.
- Bilirubin metabolism – Red blood cells break down into a substance called bilirubin. If the body has problems with bilirubin removal, it causes jaundice, a yellowish discoloration of the skin, and whites of the eyes.
- Immune function – The liver neutralizes harmful microorganisms when they reach it with the blood. That way, it neutralizes infections.
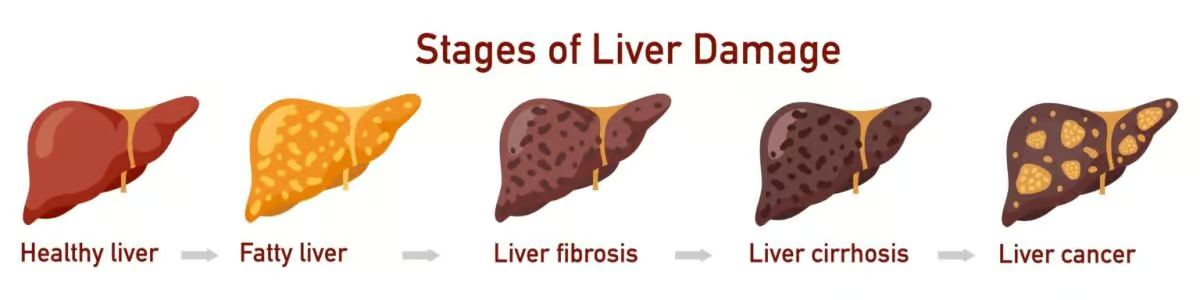
Stages of Liver Disease
Liver disease has four main stages:
- Fatty liver
- Liver fibrosis
- Cirrhosis of the liver
- Liver failure
Fatty Liver is the first stage of liver disease in which fat cells accumulate excessively. If it progresses, liver fibrosis occurs in abnormal amounts of scar tissue in the liver due to long-lasting inflammation. Fatty liver and liver fibrosis are reversible stages of liver damage.
However, fibrosis can progress into cirrhosis of the liver, the disorder in which fibrosis reaches such intensity that the scar tissue destroys the typical structure of the liver. Cirrhosis of the liver is irreversible since the damage done to the organ is major. When cirrhosis of the liver occurs, it significantly increases the risk of developing liver cancer.
Once scar tissue replaces healthy liver tissue, it can’t function properly. That poses a great problem since the liver is highly significant for proper body functioning. If the scarring reaches a point where the organ can’t work, it’s called liver failure. Then, the only remedy is a liver transplant, as replacing the damaged organ with a healthy one is the only hope for recovery.
Types
There are a few types of fatty liver disease. Distinguishing between different kinds of disease is essential because they differ in the risk of progression to more severe forms of liver disease as well as in treatment.
Nonalcoholic Fatty Liver Disease
Nonalcoholic fatty liver disease (NAFLD) is a fatty liver disease not caused by alcohol abuse, chronic use of drugs that cause fatty liver disease, or congenital genetic diseases. Nonalcoholic fatty liver disease stands as the most common chronic liver disease and holds the top position as the primary cause of abnormal liver function test results.
The leading role in the development of NAFLD is played by insulin resistance and dysregulation of the hormone that regulates the body’s energy balance. The causes include an unhealthy diet rich in carbohydrates, saturated fats, and sweetened drinks, which, together with low physical activity, leads to overweight and obesity. Genetic predisposition also plays a role.
Usually, the disease does not cause any symptoms and is accidentally diagnosed during an ultrasound examination or after abnormally high levels of liver enzymes are detected in the blood.
Alcohol-related Fatty Liver Disease
In alcohol-related fatty liver disease, the cause of the disease is excessive alcohol consumption. When you drink alcohol, the liver filters it, and every time, some of its cells get damaged. Usually, the liver can regenerate itself and replace damaged cells with new ones. But when you drink too much alcohol, liver damage may exceed its regeneration capacity, causing fatty liver disease.
Alcohol-related fatty liver disease usually doesn’t cause any symptoms until the disease is severely advanced. Then, symptoms include vomiting, weight loss, yellowing of the skin and whites of the eyes, ascites (water buildup in the abdomen), and bloody vomit.
If you drink alcohol excessively, you should tell your physician about it to check your liver’s condition.
Nonalcoholic Steatohepatitis (NASH)
Nonalcoholic steatohepatitis is a fatty liver with chronic and progressive inflammation of the liver, which, if left untreated, leads to fibrosis, cirrhosis, and liver cancer. The risk of progression to further liver disease stages is higher in NASH than in NAFLD. In this type of disease, treatment options include a few medications that aim at protecting against further liver damage.
Causes
Fatty liver disease may occur as a result of the toxic effects on the liver of various factors, such as:
- Alcohol – this is known as alcoholic fatty liver disease
- Medications– antibiotics, vitamins (vitamin A in large doses), some anticonvulsants, and certain types of anti-arrhythmic medications
- Chemical substances
- Toxins contained in mushrooms
- Obesity, starvation, protein malnutrition
- Diabetes
- Hyperadrenocorticism
- Hyperlipidemia
- Metabolic disorders
- Long-term parenteral nutrition
- Infectious diseases: hepatitis C, hepatitis D, typhoid fever
- Reye’s syndrome
- Pregnancy complications: acute fatty liver of pregnancy, eclampsia
Steatosis can also occur without the action of one specific toxic factor. Then, it is nonalcoholic fatty liver disease. The origins of this condition stem from an unbalanced diet high in saturated fats, coupled with insufficient physical activity, resulting in weight gain and obesity.
Risk Factors
You have a higher chance of getting fatty liver if you:
- Drink alcohol excessively
- Have type 2 diabetes
- Are overweight or obese
- Have insulin resistance (present in such conditions as polycystic ovary syndrome)
- Have hypothyroidism
- Have high cholesterol
- Have hypertension (high blood pressure)
- Are smoking
- Are over 50
- Have pre-existing liver abnormalities, such as hepatitis C
Symptoms
Fatty liver disease usually does not cause symptoms. Some people may experience the following:
- Fatigue
- Weakness
- General malaise
- Abdominal pain or fullness in the upper right side of the abdomen
Fatty liver disease is often diagnosed accidentally during an ultrasound examination for another reason or after abnormal liver enzyme activity is detected in the blood.
Some people may experience symptoms of liver failure – this happens if complications of fatty liver disease have already developed, e.g., liver cirrhosis:
- Unexplained weight loss
- Loss of appetite
- Yellowing color of the skin and whites of the eyes
- Edema, which is swelling, typically of your legs and hands
- Ascites, which is a water buildup in your abdomen
- Bleedings
Diagnosis
Fatty liver doesn’t usually cause any symptoms. For this reason, your physician may be the first to notice it during examination and tests for another reason. The first indication may be elevated levels of liver enzymes or changes in the ultrasound examination.
In making a diagnosis, your doctor may take the following steps:
- Taking your medical history – They can ask you about your other medical conditions, medications you take, how much alcohol you drink, and your diet.
- Blood test – Liver enzymes are alanine transaminase (ALT) and aspartate transaminase (AST). When they are elevated, it indicates that the liver is injured. Other blood tests assessing liver function include bilirubin, total protein, albumin, ALP, and prothrombin time (PT).
- Physical examination – during the examination, the physician checks for signs of liver enlargement, pain, or jaundice, such as yellow skin and whites of the eyes.
- Scans – The scans that your physician may perform include ultrasound, CT (computed tomography), and MRI. Besides usual ultrasound, there is a specific type of scan called liver ultrasound elastography, which allows physicians to monitor the progression of the liver disease.
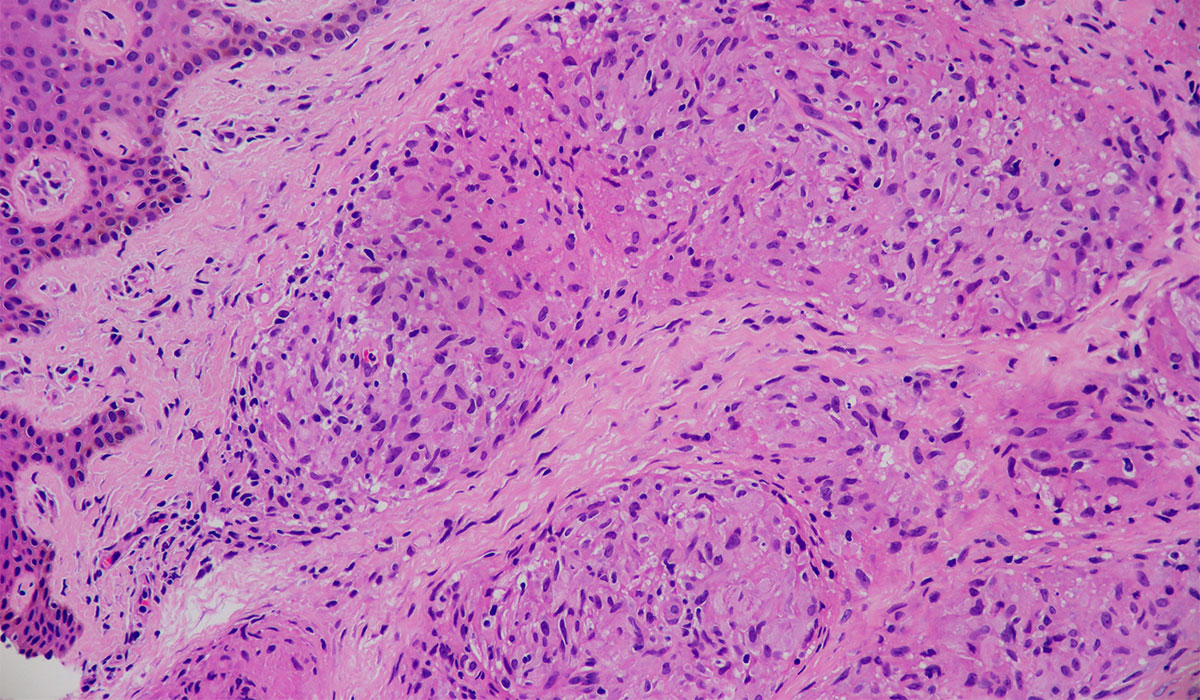
- Liver biopsy – in rare cases, a tissue sample from the liver is collected by the needle and examined under a microscope to determine the liver disease stage.
Treatment
Treatment depends on the cause of fatty liver disease. If steatosis is the result of the toxic effects of a specific substance, discontinuation of exposure usually causes remission of the disease. Alcoholic fatty liver disease usually resolves within a few weeks after cessation of alcohol consumption and slowly progresses to hepatitis and cirrhosis if continued.
The treatment of nonalcoholic fatty liver disease mainly involves lifestyle modification and, in the case of NASH, drugs that protect the liver from liver disease progression.
Medications
Currently, there is no specific medication for fatty liver disease. However, for NASH (nonalcoholic steatohepatitis), there are two medications approved by the experts: an antioxidant – vitamin E, and a drug that decreases the levels of sugar in the blood and is also used in diabetes treatment.
However, not everyone can benefit from those drugs, and you should never start therapy on your own. If you have confirmed NASH, you can talk with your physician about possible drug therapy. Still, the doctor’s decision to either start the treatment or not is based on the benefit-risk ratio, as every medication has associated side effects.
In addition, medications to treat conditions, such as high blood pressure, high cholesterol, or diabetes associated with the disease are essential.
Lifestyle Modifications
The primary treatment method for fatty liver is lifestyle modification. Your physician may recommend some changes you should introduce to your life. These include:
- Cutting alcohol consumption – If you have fatty liver, you should strictly avoid alcohol. Even if your disease has not been associated with too much alcohol drinking, you should stay clear of it to improve your liver condition.
- Diet – Experts recommend eating a healthy, balanced diet when suffering from fatty liver disease. The basis of the diet should be vegetables, fruits, whole grain products, legumes, poultry, nuts, seeds, dairy products, and eggs. Including fish in the diet is also essential since they are a source of unsaturated fat.
- Physical activity – regular physical activity of moderate intensity should be done at least 150 minutes a week. Even if it doesn’t lead to losing weight, it can improve your liver condition. Exercises you can try include walking, cycling, or swimming.
- Losing weight – keeping a BMI between 18.5 and 24.9 is advised by experts. Losing 10% of your weight causes some fat from your liver to be removed.
- Hepatitis A and B vaccination – Hepatitis A and hepatitis B viruses threaten people with already existing liver diseases, so people with fatty liver should prevent it by getting vaccinated.
- Stopping smoking

Liver Transplant
Fatty liver can progress to cirrhosis. Then, the liver may stop functioning, and a liver transplant can be necessary. In that case, your provider puts you on the waiting list, or you can receive part of the organ from a living donor. This is possible due to the liver’s exceptional ability to regenerate itself. The transplanted section and the donor’s remaining part of the liver can grow to regular sizes.
Complications
Untreated fatty liver may progress into:
- Inflammation
- Liver fibrosis
- Cirrhosis of the liver
- Liver failure
- Liver cancer
People with fatty liver disease are also at higher risk of developing heart disease.
Prevention
Preventing alcoholic fatty liver disease is not drinking too much alcohol. Since nonalcoholic fatty liver disease development is associated with obesity, diabetes, insulin resistance, or high blood cholesterol levels, it is worth implementing a healthy diet and physical activity as preventive measures. You should follow a well-balanced diet and avoid eating products with high saturated fat content and fast food. Sustaining a healthy weight is crucial for minimizing the likelihood of developing fatty liver disease. Changing your lifestyle can bring many beneficial effects, such as weight loss, which is very important in the case of overweight or obesity.
Sources
- Nassir F, Rector RS, Hammoud GM, Ibdah JA. Pathogenesis and Prevention of Hepatic Steatosis. Gastroenterol Hepatol (N Y). 2015 Mar;11(3):167-75. PMID: 27099587; PMCID: PMC4836586.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4836586/ - John Hopkins Medicine Liver: Anatomy and Functions
https://www.hopkinsmedicine.org/health/conditions-and-diseases/liver-anatomy-and-functions - National Library of Medicine (NIH) Catiele Antunes; Mohammadreza Azadfard; Gilles J. Hoilat; Mohit Gupta. Fatty Liver (2023)
https://www.ncbi.nlm.nih.gov/books/NBK441992/ - National Health Service (NHS) Non-alcoholic fatty liver disease (NAFLD) (2022)
https://www.nhs.uk/conditions/non-alcoholic-fatty-liver-disease/ - National Health Service (NHS) Alcohol-related liver disease (2022)
https://www.nhs.uk/conditions/alcohol-related-liver-disease-arld/ - Kolaric TO, Nincevic V, Kuna L, Duspara K, Bojanic K, Vukadin S, Raguz-Lucic N, Wu GY, Smolic M. Drug-induced Fatty Liver Disease: Pathogenesis and Treatment. J Clin Transl Hepatol. 2021 Oct 28;9(5):731-737. doi: 10.14218/JCTH.2020.00091. Epub 2021 Sep 14. PMID: 34722188; PMCID: PMC8516847.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8516847/ - Gherlan GS. Liver ultrasound elastography: More than staging the disease. World J Hepatol. 2015 Jun 28;7(12):1595-600. doi: 10.4254/wjh.v7.i12.1595. PMID: 26140079; PMCID: PMC4483541.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4483541/ - National Library of Medicine (NIH) Vasimahmed Lala; Muhammad Zubair; David A. Minter. Liver Function Tests (2023)
https://www.ncbi.nlm.nih.gov/books/NBK482489/ - National Library of Medicine (NIH) Ashish Sharma; Shivaraj Nagalli. Chronic Liver Disease (2023)
https://www.ncbi.nlm.nih.gov/books/NBK554597/ - Hazeldine S, Hydes T, Sheron N. Alcoholic liver disease – the extent of the problem and what you can do about it. Clin Med (Lond). 2015 Apr;15(2):179-85. doi: 10.7861/clinmedicine.15-2-179. PMID: 25824072; PMCID: PMC4953739.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4953739/ - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Nonalcoholic Fatty Liver Disease (NAFLD) & NASH (2021)
https://www.niddk.nih.gov/health-information/liver-disease/nafld-nash - Glass LM, Dickson RC, Anderson JC, Suriawinata AA, Putra J, Berk BS, Toor A. Total body weight loss of ≥ 10 % is associated with improved hepatic fibrosis in patients with nonalcoholic steatohepatitis. Dig Dis Sci. 2015 Apr;60(4):1024-30. doi: 10.1007/s10620-014-3380-3. Epub 2014 Oct 30. PMID: 25354830.
https://pubmed.ncbi.nlm.nih.gov/25354830/