Long-lasting inflammation may weaken the esophageal wall and deteriorate blood supply, forming erosions and ulcers. Over time, the affected mucosa becomes necrotic, a fistula (connection) with large vessels adjacent to the esophagus develops, and the damaged wall becomes perforated. Regardless of the causes, the course and symptoms are similar in each type of esophagitis.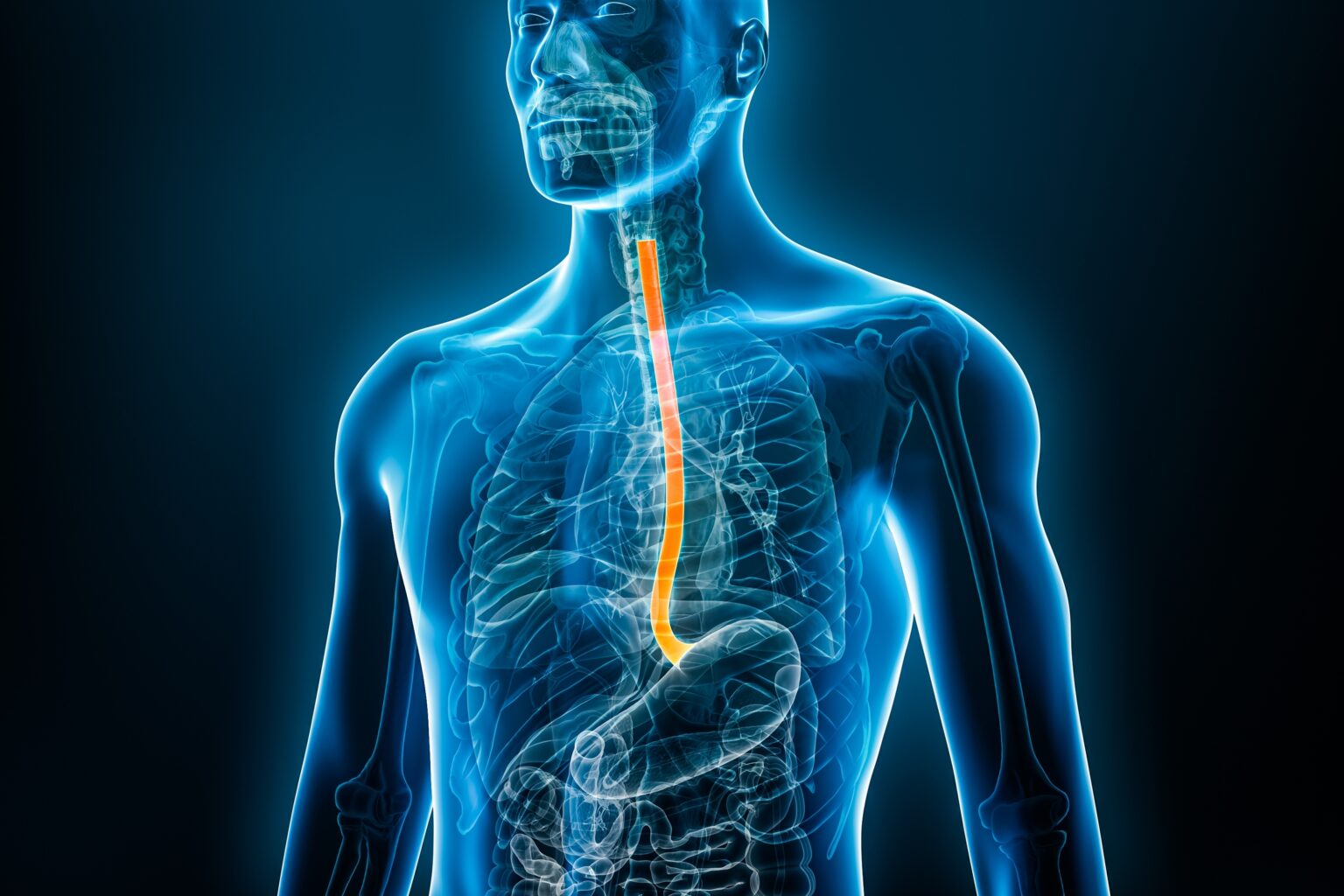
Esophagus – General Information
The esophagus is a longitudinal muscular tube. It connects the throat to the stomach and is part of the digestive system. Its function is mainly to transport food from the mouth to the stomach.
The esophageal wall consists of four layers:
- The mucous membrane, which has a folded structure and is covered with epithelium
- Submucosa
- Muscular layer
- The outer layer called the adventitia
The anatomy of the esophagus includes various types of muscles, which change smoothly as they move down the digestive tract. The upper part is dominated by striated muscles, similar to those found in the mouth and throat.
In the middle section, the structure of the human esophagus changes. Striated muscles gradually transform into smooth muscles, typical for the ducts, respiratory and urogenital systems. That kind of muscle consists of two layers, circular and longitudinal, and can remain in contraction for a long time. In this section of the esophagus, striated and smooth muscles are present, while only the latter are in the lower part.
The esophagus has upper and lower esophageal sphincters:
- The upper esophageal sphincter is a circular muscle that separates the pharynx from the esophagus
- The lower esophageal sphincter (LES) is a circular smooth muscle that prevents stomach contents from flowing back into the esophagus. In a healthy person, it is mainly in a state of contraction and relaxes when food is swallowed. The failure of the lower esophageal sphincter causes gastroesophageal reflux (GERD), which is the backflow of acidic stomach contents into the esophagus. However, in a situation of increased tension of the lower esophageal sphincter and noncomplete muscle relaxation during swallowing, esophageal achalasia develops – food that does not pass into the stomach stays in the esophagus, causing it to dilate.
In the human body, the esophagus serves purely transport functions. No significant processes take place in this section of the digestive system. Food fragments are neither crushed there (the mouth performs this function) nor digested (this process occurs below, in the stomach and intestines). Nutrients are also not absorbed into the body through the esophagus (which takes place mainly in the intestines).
Have you ever wondered how the food from your mouth is moved to your stomach? The esophagus performs the last phase of swallowing, which is entirely automatic and independent of will. The pieces of pre-crushed food are carried in the esophagus partially due to the force of gravity but mainly due to muscle contractions and the slippage provided by the mucus accumulating in the folds of the mucous membrane.
When food reaches the end of the esophagus, temporary relaxation of the lower esophageal sphincter allows the swallowed contents to enter the stomach, and its tightening prevents gastric juices and acidified contents from escaping in the opposite direction.
Types
Depending on the cause, there are a few different types of esophagitis. These include:
Reflux Esophagitis
This is the most common type of esophagitis caused by gastroesophageal reflux disease (GERD). It happens when the acidic content of the stomach backflows into the esophagus due to insufficiency of the lower esophageal sphincter. The stomach lining is covered with mucous that protects it from damage from acidic content. The esophagus, however, is not adapted this way, so when its lining has contact with stomach acid, it irritates and causes inflammation.
This type of esophagus inflammation also happens more frequently in people who often vomit, for example, people with bulimia nervosa.

Drug-induced Esophagitis
Another name for this condition is pill-induced esophagitis. Some medications may damage the lining of the esophagus by creating an alkaline or acidic environment inside it. Drug-induced esophagus inflammation may go away on its own, but in some cases, it can persist for a long time, leading to complications, including strictures of the esophagus. The medications that can cause drug-induced esophagitis include:
- Some antibiotics
- Non-steroidal anti-inflammatory drugs NSAIDs, including aspirin
- Bisphosphonates, which are drugs used in bone disease treatment, such as osteoporosis or Paget’s disease of bone
- Paracetamol
- Some anticoagulants, which are drugs used in blood clot prevention
- Chemotherapy
- Ascorbic acid
A specific group of treatments that can lead to drug-induced esophagitis is thoracic radiotherapy. Radiation therapy that targets your chest or throat can cause inflammation of the esophagus mucosa, which may cause troublesome symptoms. However, This type of inflammation is usually a temporary reaction that goes away.
Eosinophilic Esophagitis
Eosinophilic esophagitis is the second most common form of esophagitis. Eosinophils are a part of the immune system – a type of white blood cell that plays an essential role in fighting parasites and allergens. Eosinophiles are typically not present in the esophagus wall. Sometimes, however, there’s a glitch in your immune system, and it sends too many eosinophils to the esophagus to fight a potential threat (such as an allergen) that it detected. Eosinophiles accumulate in the esophagus wall, causing inflammation even when the potential danger passes.
This type of esophagitis is a chronic immune disease caused by immune system hypersensitivity. It most often affects people with other immune diseases, such as asthma, atopic dermatitis (eczema), or allergic rhinitis.
Infectious Esophagitis
Infectious esophagitis happens to people with weakened immune systems. Those include people infected with HIV infection, patients going through radiotherapy, or people after transplants. In people whose immune systems work correctly, infectious inflammation of the esophagus happens extremely rarely.
Infections of the esophagus are usually fungal or viral. Microorganisms that are responsible most often for esophagus infections include:
- Yeast infection – Candida albicans
- Cytomegalovirus (CMV)
- Oral human papillomavirus (HPV)
- Herpes simplex virus 1 (HSV1)
Treatment of infectious esophagitis differs from treatment of other types of esophagus inflammation. Yeast infections are treated with antifungal drugs, and viral infections must be differentiated, whether caused by herpes virus or cytomegalovirus, to be treated according to the infectious factor.
Causes
Esophagitis happens when the immune system is activated to fight some triggering factor in the esophagus or when the specific factor irritates tissues. Depending on the type of esophagus inflammation, various factors can trigger the inflammation of esophagus tissues. Causes of esophagitis include:
- Gastroesophageal reflux disease (GERD)
- Fungus
- Virus
- Certain medications
- Autoimmune disease
- Allergy
- Radiation
Risk Factors
Some people are at a higher risk of acquiring esophagitis. The risk factors of esophagus inflammation include:
- Having gastroesophageal reflux disease (GERD)
- Having hiatal hernia, which is bulging of the part of the stomach above the diaphragm
- The weakened immune system, for example, people with AIDS, people after organ transplant, or patients going through cancer treatment
- Radiotherapy
- Having autoimmune diseases, e.g., asthma or eczema
- Having bulimia nervosa
- Being diabetic
- Being overweight or obese
- Taking certain medications, such as NSAIDs or bisphosphonates
Symptoms
Symptoms of esophagitis include:
- Heartburn
- Swallowing difficulties
- Chest pain
- Regurgitations
- A sore throat
- Hoarseness
- Cough
- Nausea
- Vomiting
- Shortness of breath
- Burping
- The feeling of food getting stuck in the throat
- Indigestion
- Mouth sores
- Blood in vomit
- In children, you may notice feeding difficulties
- Weight loss
- Bad breath
Be vigilant of alerting signs that could indicate a more significant health concern, like cancer, when combined with the symptoms above. Such alarming cues include unexplained speedy weight reduction, nocturnal sweating, bleeding in your digestive system, and feeling weak.
Diagnosis
Determining if someone has esophagitis often involves taking a detailed medical history and conducting a thorough physical exam. Sometimes, it may be necessary to perform additional diagnostic tests to properly diagnose the cause and determine the advancement of the disease:
- Blood tests
- Gastroscopy with biopsy – during that test, the doctor inserts a flexible tube through your mouth into your esophagus and sees the inside on the screen, making it possible for them to assess your esophagus lining. Taking a small sample of your esophagus tissue (biopsy) enables the assessment of the etiology of the inflammation during examination under the microscope.
- Esophageal manometry, i.e., measurement of pressure in the muscle-lower esophageal sphincter
- Esophageal pH test, which measures the acidity level of gastric contents in the esophagus for 24 hours
- Chest X-ray allows the assessment of esophageal motility and the diagnosis of pathological changes.

Treatment
Treatment of esophagitis looks different depending on its cause. However, some medications are used to manage esophagus inflammation regardless of its etiology. These include:
- PPIs – proton pump inhibitors, medications that reduce stomach acid production.
- H2 blockers – these drugs limit the secretion of hydrochloric acid by blocking the histamine receptor on the surface of the stomach cell.
Regarding eosinophilic esophagitis, corticosteroids (anti-inflammatory drugs) and an elimination diet that eliminates allergic factors are essential. In the case of infectious inflammation, antiviral drugs (for CMV or HIV inflammation), antibiotics (for bacterial inflammation), and antifungal medications are necessary. Drug-induced inflammation management involves consulting a doctor, changing the form of the used drug, consuming it with food, and drinking plenty of water.
Apart from medications, lifestyle modifications are advised during esophagitis. It would be best to avoid fatty or spicy meals as they might further irritate the esophagus lining. Eating smaller meals and keeping the head of the bed elevated are also advised.
Complications
Complications of esophagitis include:
- Bleeding – Inflammation of the esophagus causes its tissues to be more fragile. Then, it is much easier to damage the esophageal lining and cause bleeding.
- Esophagus stricture – Chronic inflammation of the esophagus may lead to scar tissue formation. Scar tissue causes narrowing of your esophagus, otherwise called stricture. A narrowed esophagus causes swallowing difficulties, which, if severe, may lead to malnutrition and weight loss.
- Barret’s esophagus – When stomach acid backs up into the esophagus in reflux esophagitis, it can cause damage to the lining. In response, your body may try to protect itself by altering the damaged coating with one much like what you’d find inside your intestines – thus giving rise to Barrett’s Esophagus. This condition is pre-cancerous and poses an increased risk of developing cancer of the esophagus later on.
- Perforation – Long-lasting inflammation may lead to ulcer (open sores) formation inside the esophagus. Suppose the ulcer persists for a long time. In that case, it may further destroy the esophageal lining, and if it destroys the entire thickness of the esophageal wall, perforation (puncture) of the esophagus may occur.
- Aspiration pneumonia – Aspiration pneumonia is caused by the aspiration of food into the respiratory tract. During esophagitis, there is a risk of food entering the respiratory tract, especially if the esophagitis is associated with gastroesophageal reflux and lower esophageal sphincter failure.
- Laryngitis – If the lower esophageal sphincter works incorrectly, the stomach’s acidic content can regurgitate into the respiratory system and irritate the larynx, causing inflammation.
Prevention
The key to preventing esophagitis is a modification of lifestyle and diet.
You should avoid dietary habits and food triggers that may induce esophagitis, including fatty and spicy meals, coffee, chocolate, alcohol, smoking, and a short time between dinner and bedtime.
If you are diagnosed with eosinophilic esophagitis, you should avoid foods you are allergic to. If you suspect that you suffer from nocturnal acid reflux (you have symptoms like sore throat in the morning, night cough, and voice hoarseness), try elevating the head end of the bed. If your bed cannot be regulated, try putting a wedge under your mattress.
If you are overweight, losing a few pounds is advised, as obesity is a significant risk factor for esophagitis. It would be best to remember that even simple things like taking smaller bites, chewing your food thoroughly, and avoiding bending your stomach after a meal can significantly affect your esophagus’s health.
When Should You See a Doctor?
You should contact your physician if you notice symptoms of esophagitis, such as heartburn, chest pain, swallowing difficulties, or hoarseness. Your doctor will order proper tests and implement treatment. If you risk getting esophagitis, for example, if you have a condition associated with a weakened immune system or take medications that can cause esophagus inflammation, inform your physician about it. A doctor who specializes in gastrointestinal diseases is called a gastroenterologist.
Sources
- National Library of Medicine (NIH) Suhaib A. Bajwa; Fadi Toro; Anup Kasi. Physiology, Esophagus (2023) https://www.ncbi.nlm.nih.gov/books/NBK519011/
- National Library of Medicine (NIH) Catiele Antunes; Ashish Sharma. Esophagitis (2023) https://www.ncbi.nlm.nih.gov/books/NBK442012/
- National Library of Medicine (NIH) Samy A. Azer; Anil Kumar Reddy Reddivari. Reflux Esophagitis (2023) https://www.ncbi.nlm.nih.gov/books/NBK554462/
- National Library of Medicine (NIH) Fatima Saleem; Ashish Sharma. Drug-Induced Esophagitis (2023) https://www.ncbi.nlm.nih.gov/books/NBK549818/
- National Library of Medicine (NIH) Jordan M. Roussel; Sudha Pandit. Eosinophilic Esophagitis (2023) https://www.ncbi.nlm.nih.gov/books/NBK459297/
- Wilcox CM. Infectious Esophagitis. Gastroenterol Hepatol (N Y). 2006 Aug;2(8):567-568. PMID: 28316525; PMCID: PMC5350250. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5350250/
- Chung TH, Lee J, Jeong ID, Lee KC. Effect of Weight Changes on the Development of Erosive Esophagitis. Korean J Fam Med. 2020 Jan;41(1):14-19. doi: 10.4082/kjfm.19.0003. Epub 2020 Jan 9. PMID: 31914725; PMCID: PMC6987027. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6987027/