Body processes governed by the autonomic nervous system are functions we usually don’t give much thought about during the day. This is because they are automatic, allowing us to focus on more conscious, important things. Such processes include heart rate, digestion, kidney function, blood pressure, pupil dilation, and respiration.
Disrupting these functions can have unpredictable consequences. Some people do not notice many changes, experiencing only minor inconveniences. However, others have to learn how to manage severe symptoms such as chest pain, fainting, difficulty breathing, nausea, and many more, depending on which ANS is disrupted.
How Common Is Dysautonomia?
According to the data collected by Dysautonomia International, a non-profit organization, dysautonomia affects over 70 million people worldwide. Although some factors like heritage and family history increase the risk of it, anyone can develop it regardless of age, race, and ethnicity.
Types of Dysautonomia
Dysautonomia is classified into 15 types. Two of the most common are postural orthostatic tachycardia syndrome (POTS) and neurocardiogenic syncope/autonomic mediated syncope (NCS). Examples of other types include multiple system atrophy (MSA), diabetic autonomic neuropathy, autonomic dysreflexia (AD), and baroreflex failure.
Postural Orthostatic Tachycardia Syndrome (POTS)
Postural orthostatic tachycardia syndrome (POTS), a more common type of dysautonomia, affects 1 in 100 teenagers and affected about 3 million Americans before the coronavirus pandemic. Common symptoms include dizziness, chest pain, increased heart rate after standing up, sitting, or lying down, and shortness of breath.
Neurocardiogenic Syncope (NCS)
Neurocardiogenic syncope is another of the most common types. It affects tens of millions of people worldwide, often causing only mild symptoms. Many people with this condition faint only 1 to 2 times during their lifetime. However, a more severe version of NCS causes several faints during the day, which increases the risk of injuries due to falling.
Multiple System Atrophy (MSA)
Multiple system atrophy is a rare and severe form of dysautonomia usually observed in people over 40. It impacts involuntary movements with a tendency to get worse over time. It leads to such neurological problems as severe balance problems, dementia, tremors, and weakness.
People affected by MSA are usually bedridden within two years after diagnosis and are expected to live for 5-10 years.
Diabetic Autonomic Neuropathy
Diabetic autonomic neuropathy may develop due to diabetes. It affects the nerves that control the digestive system, genitals, heart, bladder, and other organs.
Symptoms of diabetic autonomic neuropathy include:
- Constipation
- Impaired neurovascular function
- Sweating irregularities
- Breathing problems
- Erectile dysfunction
- Gastroparesis
- Fast resting heart rate
Autonomic Dysreflexia (AD)
Autonomic dysreflexia (AD) usually develops as secondary dysautonomia in people with spinal cord injuries. The risk of AD increases with the severity of the injury. Its symptoms include nausea, blotchy skin, headaches, slow pulse, blocked nose, and goosebumps near the injury site.
Baroreflex Failure
Baroreflex failure is a rare condition that affects blood pressure. The baroreflex mechanism is responsible for maintaining correct blood pressure thanks to stretch receptors called baroreceptors situated in important blood vessels. If the function of baroreceptors is affected, blood pressure can become too high or too low, potentially leading to headaches, abnormal heart rate, and excessive sweating.
Causes
Dysautonomias can be either primary or secondary, depending on what causes them. Primary dysautonomias refer to dysautonomias that develop independently, while secondary dysautonomias occur due to other health conditions.
Primary Dysautonomias
Primary dysautonomias don’t happen as often as secondary dysautonomias. They develop without a specific condition causing it and are associated with several factors:
- Being Jewish (primarily of Ashkenazi Jewish heritage)
- Being Eastern European
- Family history of dysautonomia
You are at the greatest risk of developing dysautonomia if a first-degree family member has it.
Secondary Dysautonomias
Many medical conditions may cause or increase the risk of developing dysautonomia. Examples include the following:
- Sarcoidosis
- Multiple sclerosis and neuromyelitis optica
- Ehlers-Danlos syndrome (and other connective tissue disorders)
- Pure autonomic failure
- Lupus
- Traumatic brain injury
- Chiari malformation
- Medications or medical procedures
- ALS (Amyotrophic lateral sclerosis, often known as “”Lou Gehrig’sGehrig’s disease.”)
- Autoimmune autonomic ganglionopathy (AAG)
- Guillain-Barré syndrome
- Tetanus
- Porphyria (especially acute intermittent porphyria)
- Orthostatic hypotension
- Neuroleptic malignant syndrome
- Botulism
- Toxins, poisons, or heavy metals (like mercury, arsenic, or organophosphates found in pesticides)
- Type 2 diabetes
- Parkinson’sParkinson’s disease
- Multiple system atrophy (MSA)
- Vasovagal syncope (less commonly known as “neurocardiogenic syncope””)
- Wernicke-Korsakoff syndrome (or vitamin B1 deficiency)
- Rheumatoid arthritis
- Postural orthostatic tachycardia syndrome (POTS)
- Lewy body dementia
- COVID-19 infection (especially “long COVID,” when you have symptoms for much longer than expected)
- Brain tumors (including cancer)
- Spinal cord injury
- Stiff person syndrome
- Vitamin B12 deficiency
- Serotonin syndrome
- Complex regional pain syndrome (CRPS)
- Lyme disease
- Vasovagal syncope (less commonly known as “neurocardiogenic syncope”)
- Primary focal hyperhidrosis
Signs And Symptoms
Dysautonomia may affect various body systems, so the list of possible problems it may cause is vast. Depending on which body function is disrupted, one person with dysautonomia may experience a completely different set of issues than other affected people.
Doctors usually group dysautonomia symptoms based on the affected function of the autonomic nervous system (ANS). There are eight such groups:
- Sensory perception
- Cognition
- Heart rate
- Circulation and blood pressure
- Excretion
- Digestion
- Respiration
- Excretion
Examples of the most common problems associated with the eight ANS functions include the following:
- Fast heart rate (tachycardia)
- Slow heart rate (bradycardia)
- Nausea and vomiting
- Sexual dysfunction
- Concentration and memory problems
- Low appetite
- Fatigue and intolerance to exercise
- Disturbances in the visual field
- Problems with the gastrointestinal system
- Heart palpitations
- Sleeping problems
- Frequent urination
- Temperature regulation problems
- Disrupted sleep pattern
- Runny nose
- Vertigo
- Difficulty adjusting to light changes
- Dry or watery eyes
- Migraines or frequent headaches
- Breathing difficulties
- Mood swings
- Sweating more or less than usual
- Fast, slow, or irregular heartbeat
- Chest pain
- Low blood pressure
- Swings in body or skin temperature
- Excessive drooling
- Tremors
- An inability to stay upright
- Dizziness or lightheadedness
- Sound sensitivity
- Shortness of breath (dyspnea)
- Clammy or pale skin
- Temperature regulation problems
- Intolerance to exercise due to heart problems
- Pinpoint-eye pupils or wide-eye pupils
- Changes in bowel movements (constipation or diarrhea)
- Brain fog
- Trouble swallowing (dysphagia)
- Abdominal pain
- Acid reflux
- Impaired tear production
- Difficulty focusing
- Forgetfulness

Complications
Dysautonomia may result in many severe and life-threatening health problems. Examples of the most concerning complications include:
- Difficulty breathing
- Incontinence or urinary tract infections if kidney functions are affected
- Diarrhea, constipation, and other gastrointestinal problems if digestion is affected
- Fainting
- Heart beating too fast, too slow, or irregularly
Diagnosis And Tests
Diagnosis of dysautonomia encompasses a thorough physical examination, a review of the patient’s medical and family history, and determining the type of dysautonomia and the affected functions of the autonomic nervous system.
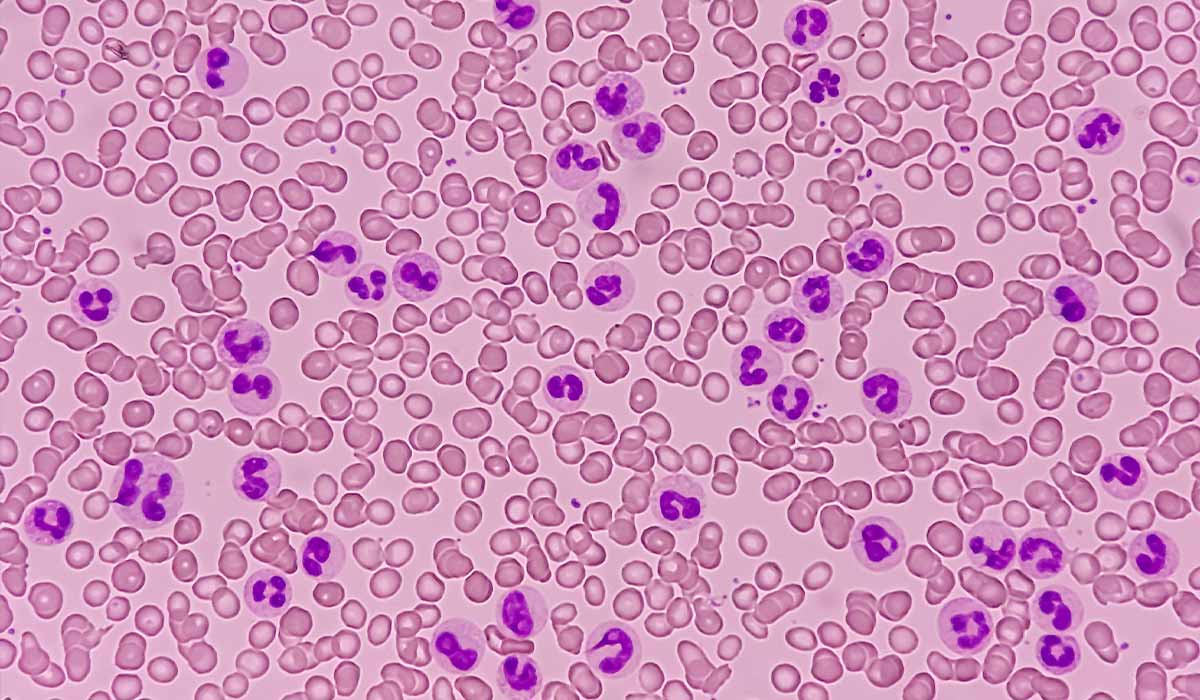
Dysautonomia often poses a diagnostic challenge and requires several tests to diagnose correctly. Some of these tests include:
- Electrocardiogram (ECG/EKG)
- Sweat tests (quantitative sudomotor axon reflex text)
- Ultrasound
- Urine analysis
- Complete blood count
- Tilt table test
- Pupil measurement testing (pupillometry)
- Spirometry
Your doctor may order additional tests depending on your specific needs. It is challenging to list all diagnostic methods used in investigating cases of dysautonomia, which stems from its unpredictable nature and the wide variety of health issues it may lead to.
Conditions Similar to Dysautonomia
Another diagnostic challenge of dysautonomia is differentiating it from other medical conditions that may mimic its symptoms. Examples of such conditions are as follows:
- Medication use
- Blood loss
- Hyperthyroidism
- Dehydration
- Anxiety disorders
- Adrenal insufficiency
- Shock
- Heart attack
- Electrolyte imbalances
- Heart arrhythmias
- Hyperglycemia
- Anemia
- Drug and alcohol abuse
- Heart disease
Treatment
There is no cure for dysautonomia, but several treatment strategies exist to relieve symptoms and help manage this condition more effectively. Treatment is usually a combination of medication to address specific health problems caused by dysautonomia, changes in daily habits, and adjustments in diet.
Medication
Some people may benefit from medication, such as drugs that increase blood pressure or immune-suppressing medications, if autoimmune conditions develop due to dysautonomia.
Ask your doctor if you should take any medication to aid you against dysautonomia. You may need to seek advice from multiple specialists, depending on which automatic functions of your body get disrupted.
Lifestyle and Diet Changes
Some of the common lifestyle and diet adjustments used to treat dysautonomia include:
- Increasing water intake to maintain blood pressure
- Adding salt to food to increase blood pressure
- Wearing sunglasses
- Physical therapy
- Sleeping with the head raised 6 to 10 inches higher than the body
- Wearing compression socks
- Avoiding triggers that make you dizzy
Your healthcare provider remains your most reliable source of information regarding dysautonomia treatments due to the many possibilities. They possess the expertise to offer details tailored to your situation and requirements. Additionally, they can inform you about potential side effects and complications and guide you in minimizing or preventing them.

Prognosis for Dysautonomia Patients
Because dysautonomia is unpredictable and can vary greatly from person to person, it is difficult to tell what life with this condition would be like. Depending on the severity of the symptoms and the affected function of the autonomic nervous system, it may be a minor or severe problem. Some people don’t experience any symptoms for months or years, while others are impacted daily.
Severe dysautonomia may limit the ability to work and perform daily activities and even lead to life-threatening complications. If you suspect you may have dysautonomia, contact a healthcare professional to receive a diagnosis. Your doctor will evaluate how much dysautonomia impacts your life and provide a prognosis based on your case.
When Should You Seek Emergency?
Dysautonomia may cause severe symptoms that make you want to contact a medical emergency. Sometimes, it may be difficult to tell if dizziness, lightheadedness, or breathing difficulty are caused by dysautonomia or if they occurred due to other health problems. When you are experiencing a serious health issue, such as severe chest pain, difficulty breathing, or heart palpitations, you should always contact an emergency, even if you are in doubt.
To avoid hesitation during a crisis, discuss with your doctor what to do when such problems arise and how to differentiate them from dysautonomia.
Dysautonomia – Key Facts You Should Know
Dysautonomia is a disorder affecting the autonomic nervous system (ANS), disrupting automatic bodily functions such as heart rate, digestion, and blood pressure. It manifests with diverse symptoms, including dizziness, chest pain, and difficulty breathing. Its complications can be severe, impacting breathing, urinary functions, gastrointestinal health, and heart rhythm.
There are various types of dysautonomia, such as postural orthostatic tachycardia syndrome (POTS), neurocardiogenic syncope (NCS), multiple system atrophy (MSA), diabetic autonomic neuropathy, autonomic dysreflexia (AD), and baroreflex failure.
Primary dysautonomias develop independently, often linked to factors like heritage and family history, while secondary dysautonomias result from underlying health conditions. Causes include genetic predisposition, certain diseases, medications, and trauma.
Dysautonomia symptoms vary widely, affecting sensory perception, cognition, heart rate, circulation, excretion, digestion, respiration, and temperature regulation.
Diagnosis involves physical exams and tests like ECG, sweat, and ultrasound. Differential diagnosis is crucial to distinguish dysautonomia from conditions with similar symptoms.
Although there’s no cure, treatment focuses on symptom management. Medications, lifestyle changes, and dietary adjustments may be recommended. Emergency medical attention is necessary for severe symptoms, such as chest pain or difficulty breathing.
Prognosis varies, with dysautonomia’s unpredictable nature making it challenging to determine the impact on an individual’s life.
Seeking professional guidance is crucial for accurate diagnosis, personalized treatment plans, and understanding the prognosis based on the severity of symptoms and affected ANS functions.
Sources
- Dysautonomia. (2019). What is dysautonomia?
https://www.dysautonomiainternational.org/page.php?ID=34 - The Dysautonomia Project. (2023). Dysautonomia.
https://thedysautonomiaproject.org/dysautonomia/ - Child Neurology Foundation. (2021). Dysautonomia.
https://www.childneurologyfoundation.org/disorder/dysautonomia/ - NIH. (2021). Dysautonomia: A Forgotten Condition – Part 1.
https://pubmed.ncbi.nlm.nih.gov/33886735/ - MedlinePlus. Autonomic Nervous System Disorders.
https://medlineplus.gov/autonomicnervoussystemdisorders.html