If an individual is a diabetic, they are either not producing enough insulin or the existing insulin isn’t practical. That way, too much sugar stays in your blood, causing symptoms and complications of diabetes.
The full name of diabetes is diabetes mellitus – mellitus, a Latin word that means “sweet as honey” and refers to the significant symptom of diabetes – high blood sugar levels.
Types of Diabetes
There are several types of diabetes. Everyone who suffers from diabetes has a heightened blood sugar concentration (hyperglycemia). However, the causes of this elevation and the methods of treating it may differ, depending on the kind of diabetes. Experts distinguish:
- type 1 diabetes,
- type 2 diabetes,
- gestational diabetes,
- LADA diabetes (Latent Autoimmune Diabetes in Adults),
- MODY diabetes (Maturity Onset Diabetes of the Young).
Type 1 Diabetes
Type 1 diabetes accounts for about 10% of all types of diabetes. It used to be called insulin-dependent diabetes or juvenile diabetes due to its development mechanism and the age at which the disease is most often diagnosed. The onset of the illness usually falls between the ages of 10 and 14.
Type 1 diabetes is caused by the almost absolute destruction of the pancreas’s insulin-producing cells (so-called beta cells). The immune system starts manufacturing antibodies that start destroying pancreas cells for an unexplained cause. Damaged cells can no longer produce insulin, leading to sugar accumulation in the bloodstream.
Primary symptoms of type 1 diabetes are usually very characteristic and severe, which result from very high blood sugar levels.
Type 1 diabetes is not inherited, but people with type 1 diabetes are genetically predisposed to other autoimmune diseases. There are no treatments that can prevent type 1 diabetes.
The treatments necessary for type 1 diabetes involve the introduction of insulin from the outside of the body, either through numerous injections or with an insulin pump. Insulin is an extremely important hormone that all living organisms need to survive, and people with type 1 diabetes need to take it from the outside. It must be administered several times a day, including before each meal.
Type 2 Diabetes
Type 2 diabetes is also known as non -insulin- dependent or adult -onset diabetes. The most prevalent form of diabetes is type 2 diabetes. Experts estimate that around one in ten adults has type 2 diabetes.
Type 2 diabetes has two main causes: reduced insulin production, which is caused on by a number of genetic factors and body cells becoming resistant to the impact of insulin, which can be driven on by both genetic and environmental (such as obesity) factors.
At the time of diagnosis, the pancreas of persons with type 2 diabetes typically makes insulin. However, either there isn’t enough of it to maintain the correct blood sugar level, or the insulin is ineffective due to a condition known as insulin resistance. Insulin resistance is the reduced sensitivity of body tissues to the action of insulin.
Because in this type of diabetes, the problem is not a lack of insulin but its malfunction, the symptoms of the disease are mild and often do not occur at first. Type 2 diabetes is usually determined when a person has higher than normal glucose levels which can commonly be found out by chance when someone undergoes screening. However, this does not mean that it is a less severe disease. If left untreated, long-term injury to the body can occur even though signs and symptoms may not initially be present.

LADA Diabetes (Latent Autoimmune Diabetes in Adults)
LADA is a specific type of type 1 diabetes that occurs when the immune system attacks the insulin-producing pancreas cells. The immune system creates antibodies which target pancreatic cells and cause their destruction. Unlike type 1 diabetes, where symptoms appear suddenly, LADA diabetes develops over the years, and blood glucose levels rise gradually. It can occur at any age but generally between ages 30 – 70. Patients with LADA type diabetes are average or slightly overweight, do not have a family history of diabetes, but often suffer from another autoimmune disease (hyperthyroidism or hypothyroidism, celiac disease).
MODY Diabetes (Maturity Onset Diabetes of the Young)
MODY diabetes, or Maturity Onset Diabetes of the Young, is a rare type of diabetes (about 2% of all cases) that is caused by an inherited gene mutation. It occurs at a young age, which is typical of type 1 diabetes, while the course of the disease is similar to type 2 diabetes. No connection exists between this specific kind of diabetes and being overweight or obese.
Gestational Diabetes
Gestational diabetes is a particular type of diabetes. It occurs in about 10% of pregnancies.
During pregnancy, there is an increase in the concentration of certain hormones (estrogens, progesterone, placental lactogen, and prolactin). These hormones act as insulin antagonists, blocking insulin action on tissues and decreasing body cells’ sensitivity to insulin. Hence the rise in blood glucose.
Gestational diabetes is when blood glucose levels remain elevated during pregnancy. It appears only in women that were not diagnosed with diabetes before pregnancy. This disorder resolves after delivery.
Symptoms of gestational diabetes usually do not appear. Laboratory tests are the only way to identify high glucose levels in the blood. For this reason, it is absolutely essential for every pregnant woman to go for regular check-ups.
An oral glucose tolerance test is used to diagnose gestational diabetes. It should be taken while fasting and is composed of several stages. The first step is a blood test for fasting glucose. Then the pregnant woman must drink a solution containing 75 grams of glucose. The woman is requested to rest seated and return for a blood draw after 60 and 120 minutes. This medical procedure is carried out on females between 24 and 28 weeks gestation. However, a physician can request this examination sooner if the woman is at an increased danger of getting diabetes.
Gestational diabetes goes away after delivery. It is worth noting, however, that pregnant women who have had gestational diabetes are at risk of developing it in the future.
Sometimes, blood sugar amounts do not go back to their usual levels after the birth of a baby. This does not mean that the mother had gestational diabetes, but that regular diabetes was found out unexpectedly during her pregnancy. In such a situation, it is necessary to continue treatment for life.

Symptoms
How do you know you may have diabetes? The most common symptoms of diabetes include:
- excessive thirst
- dry mouth
- increased hunger
- sudden weight loss
- frequent peeing
- bedwetting
- weakness, easy fatigability
- irritability, difficulty concentrating
With a long-term course of diabetes, you can observe the following:
- slow wound healing
- recurrent skin infections
- tingling in the palms of the hands and soles of the feet
- vision deterioration
- inflammation of the gums
- swelling.
Testing
Diabetes diagnosis and monitoring tests include:
- Measuring blood sugar from a pricked finger with a device called a glucometer, which is the primary method of self-monitoring in patients already diagnosed with diabetes
- Oral glucose tolerance test (OGTT). In this test, the nurse draws blood on an empty stomach, after which you have to drink a solution of 75 grams of glucose and wait 2 hours, after which the nurse draws blood again for blood sugar testing. In some people, such as pregnant women, the testing scheme includes checking the blood glucose level twice: one hour and two hours after drinking the prepared solution. A correct test result is a blood sugar below 140 mg/dL after 2 hours, and a blood glucose level ≥ 200 mg/dL after 2 hours indicates diabetes.
- Fasting glucose level test (the correct result is 70-99 mg/dl)
- Urine test. People with diabetes can have sugar in their urine, which is conducive to urinary tract infections.
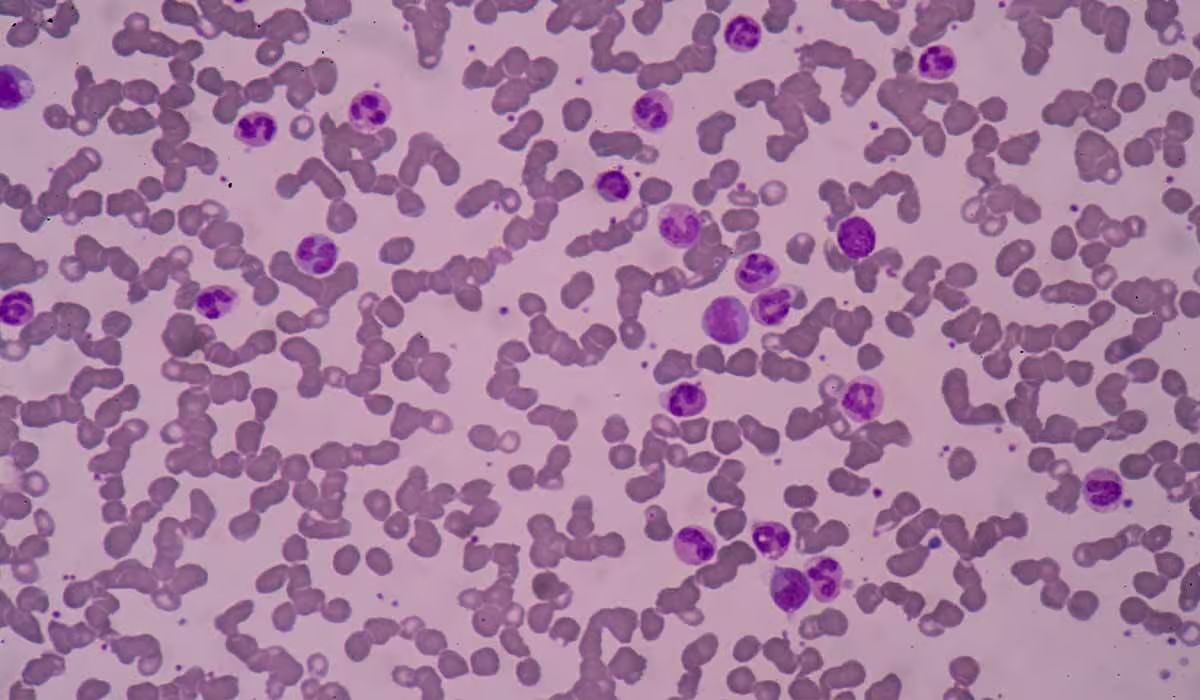
- Measurement of glycated hemoglobin HbA1C, this test gives information about the average blood sugar level over the last 2-3 months, thanks to which, apart from diagnosing diabetes, doctors also use it to monitor the effectiveness of its treatment.
Treatment
Diabetes is a chronic disease that requires ongoing treatment and monitoring. Diabetes treatment is aimed at getting your blood sugar to normal.
Medications
A doctor may recommend using different medications to help manage type 2 diabetes. These drugs can work in a range of ways such as improving how cells respond to insulin, enhancing the production of insulin, stifling the absorption of sugars from the digestive system, or increasing the elimination of sugar in the urine.
Insulin
Individuals diagnosed with type 1 diabetes necessitate the use of insulin as a form of treatment. In type 2 diabetes, gestational diabetes, and other less common types of diabetes, insulin is also sometimes used, but not in every case.
Insulin is given as subcutaneous injections several times a day. Insulin is administered into the belly but can also be delivered into the side of the thigh and the back of the upper arm. Short needles of 4 to 8 millimeters in length are used for injection. Insulin must be administered before each meal, and the amount of insulin given before a meal is calculated based on the amount of carbohydrates in it.
Insulin Pump
An insulin pump is a form of treatment in which a person with diabetes is constantly connected to a device that mimics the work of the pancreas. The insulin pump has a reservoir with insulin and releases it into the blood in small portions throughout the day and in larger doses before meals.
Individuals who have type 1 diabetes can benefit from using an insulin pump. Rather than having to take insulin injections many times a day, this approach to treatment can enhance their daily living.
Diet and Physical Activity
In treating diabetes (especially type 2 diabetes), it is vital to maintain a healthy weight, introduce a healthy diet and get regular physical activity.
The diabetic diet is based on the basic principles of healthy eating. Its purpose is to prevent rapid fluctuations in blood sugar levels.
In the diet of people who have diabetes, experts recommend:
- vegetables, including tomatoes, cucumbers, green leafy vegetables, onions, peppers, cabbage, broccoli, cauliflower, celery, parsley, carrots, limited amounts of potatoes, pumpkin, corn,
- fruits low in simple sugars, e.g., strawberries, raspberries, blueberries, watermelon, citrus, cherries, plums, avocados
- wholegrain cereal products, i.e., wholegrain bread, wholegrain pasta, brown rice
- dairy products such as yogurt, buttermilk
- poultry and lean meat
- vegetable oils, e.g., rapeseed, olive oil
While contraindicated products include fatty meat, sweets, sweetened drinks, or white bread, you should also avoid drinking alcohol, which promotes the development of hypoglycemia – a common complication of diabetes.

Complications
Hypoglycemia
Hypoglycemia is a blood sugar decrease (decrease below 70 mg/dL). It is the most common acute complication of diabetes. In diabetic patients, hypoglycemia may be caused by too much insulin injected.
Symptoms of hypoglycemia include
- pale skin,
- increased sweating,
- trembling hands,
- anxiety,
- weakness,
- and, in severe cases, loss of consciousness.
Hypoglycemia is an emergency. If the sugar level is not raised in time, the patient may lose consciousness and, in extreme cases, life.
Frequent hypoglycemia can lead to serious cardiovascular issues and damage brain cells. To counter mild or moderate symptoms, one should consume sugary drinks or food with high glucose levels. Then, to prevent relapsing, a meal with complex carbohydrates like sandwiches should be eaten.
Ketoacidosis
Ketoacidosis is a serious consequence of not properly managing diabetes, often leading to life-threatening complications in patients with type 1 diabetes. Its symptoms include abdominal pain, nausea, vomiting, headaches, fatigue, excessive thirst, and frequent urination. The smell from the mouth is also characteristic, which resembles the smell of rotten apples. If left untreated, it can lead to a diabetic coma and even death.
Stroke and Heart Attack
Too much sugar in the blood damages the blood vessels, including blood vessels of the brain and heart. If high blood sugar is long-lasting, diabetes is left untreated or poorly managed; it can lead to severe complications such as a heart attack or stroke.
Diabetic Nephropathy
Diabetic nephropathy is a chronic kidney disease that develops in people with diabetes due to persistently high blood sugar levels. Kidney damage is irreversible. A urine test is the only way to detect a disease which has no initial symptoms. It is only in the advanced stage of development that disturbing symptoms appear, such as general weakness, easy tiring, swelling, high blood pressure, and gray skin color.
Vision Damage
Diabetes can damage the blood vessels and nerves in the eyes. Doctors call this condition diabetic retinopathy. Many people with diabetes do not notice changes at first. But it can eventually cause vision loss and blindness.
Nerve Damage
People with diabetes with uncontrolled blood sugar levels have an increased risk of nerve damage (diabetic neuropathy). Initially, the patient feels tingling in the feet and hands, and sensitivity to temperature or touch decreases, followed by numbness and alternating cold or hot sensations. The skin burns or itches intensely.
Diabetic Foot
The term diabetic foot refers to several pathological changes in the foot that occur due to damage to the nerves and blood vessels in diabetic patients. Typical changes and symptoms of the diabetic foot include wounds, most often located on the sole or dorsum of the foot.
Diabetic foot therapy must include local and systemic treatment at the same time. Treatment includes balancing blood sugar levels and treating infections locally and generally. Unfortunately, necrosis sometimes occurs, and the only life-saving option is amputation.
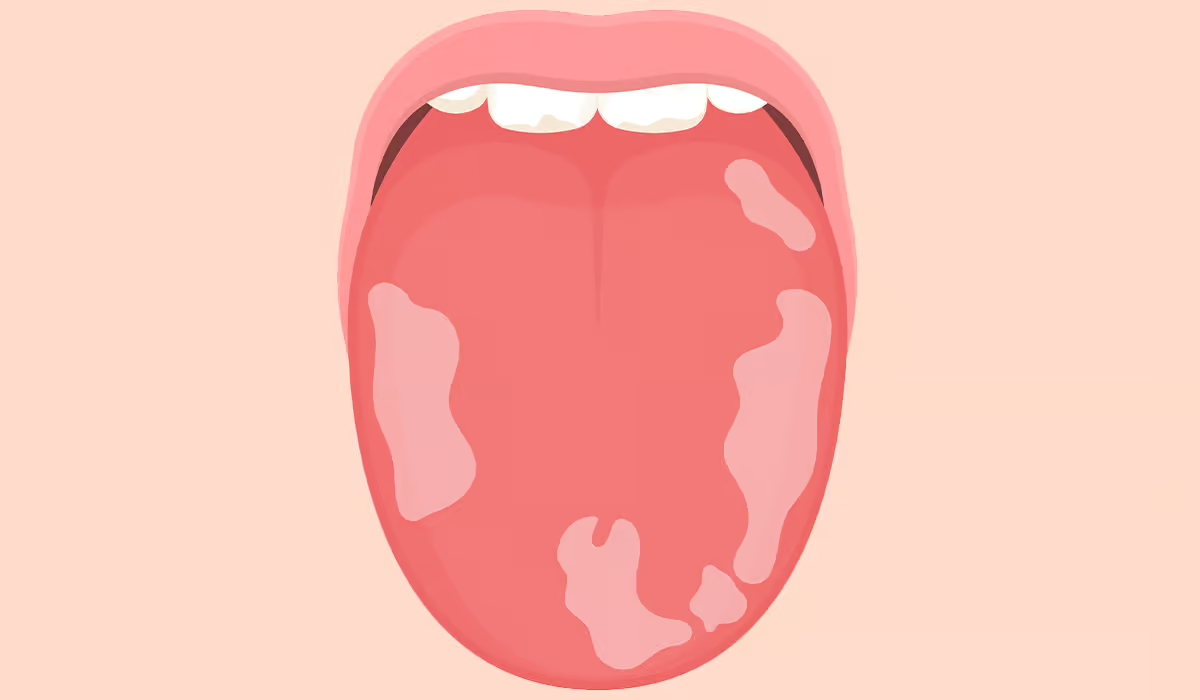
Frequent Infections
People whose diabetes is not treated correctly are at a high risk of infection due to impaired body defense mechanisms.
The presence of high blood sugar levels increases the risk of fungal infections, particularly in the mouth. During candidiasis of the oral cavity, white coatings are visible on the mucous membrane of the cheeks, tongue, and palate.
Complications of Gestational Diabetes
Gestational diabetes requires diagnosis and appropriate treatment, as it is associated with dangerous consequences such as:
- macrosomia, i.e., too much birth weight of a newborn
- fetal death
- premature birth
- recurrent urinary tract infections
- too much amniotic fluid (fluid surrounding the baby during pregnancy)
- complications in the newborn (immaturity of the respiratory system, hypoglycemia)
- childhood obesity in adolescence
Prevention
By following a balanced diet as well as participating in regular physical activity, one can prevent beginning of type 2 diabetes. Regular exercise reduces insulin resistance. A good diet and regular exercise are proven to be especially helpful in reducing the beginning of type 2 diabetes, as shown by studies.
There is currently no effective technique to prevent the onset of type 1 diabetes since it is unknown why the defense system harms the pancreatic cells in this disease.
Sources
- Amit Sapra; Priyanka Bhandari. Diabetes (2023)
https://www.ncbi.nlm.nih.gov/books/NBK551501/ - Centers for Disease Control and Prevention Type 1 Diabetes (2021)
https://www.cdc.gov/diabetes/basics/type1.html - Centers for Disease Control and Prevention Type 2 Diabetes (2023)
https://www.cdc.gov/diabetes/basics/type2.html - Galicia-Garcia U, Benito-Vicente A, Jebari S, Larrea-Sebal A, Siddiqi H, Uribe KB, Ostolaza H, Martín C. Pathophysiology of Type 2 Diabetes Mellitus (2020)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7503727/ - Venkatraman Rajkumar; Steven N. Levine. Latent Autoimmune Diabetes (2022)
https://www.ncbi.nlm.nih.gov/books/NBK557897/ - Shubrook JH, Chen W, Lim A. Evidence for the Prevention of Type 2 Diabetes Mellitus (2018)
https://pubmed.ncbi.nlm.nih.gov/30398570/ - Lende M, Rijhsinghani A. Gestational Diabetes: Overview with Emphasis on Medical Management (2020)
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7767324/ - Kc K, Shakya S, Zhang H. Gestational diabetes mellitus and macrosomia: a literature review (2015)
https://pubmed.ncbi.nlm.nih.gov/26045324/ - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Diabetes Diet, Eating, & Physical Activity (2016)
https://www.niddk.nih.gov/health-information/diabetes/overview/diet-eating-physical-activity - Johns EC, Denison FC, Norman JE, Reynolds RM. Gestational Diabetes Mellitus: Mechanisms, Treatment, and Complications (2018)
https://pubmed.ncbi.nlm.nih.gov/30297319/ - Bandyk DF. The diabetic foot: Pathophysiology, evaluation, and treatment (2018)
https://pubmed.ncbi.nlm.nih.gov/30876640/ - Pranita Ghimire; Amit S. Dhamoon. Ketoacidosis (2022)
https://www.ncbi.nlm.nih.gov/books/NBK534848/ - Unnati V. Shukla; Koushik Tripathy. Diabetic Retinopathy (2023)
https://www.ncbi.nlm.nih.gov/books/NBK560805/ - M. Luiza Caramori, MD, PhD, MSc and Peter Rossing, MD, DMSc. Diabetic Kidney Disease (2022)
https://www.ncbi.nlm.nih.gov/books/NBK279103/ - Myron A. Bodman; Matthew Varacallo. Peripheral Diabetic Neuropathy (2022)
https://www.ncbi.nlm.nih.gov/books/NBK442009/ - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Insulin, Medicines, & Other Diabetes Treatments (2022)
https://www.niddk.nih.gov/health-information/diabetes/overview/insulin-medicines-treatments - National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) Diabetes Tests & Diagnosis (2022)
https://www.niddk.nih.gov/health-information/diabetes/overview/tests-diagnosis - Rochelle Naylor, MD, Amy Knight Johnson, MS, CGC, and Daniela del Gaudio, Ph.D. Maturity-Onset Diabetes of the Young Overview (2018)
https://www.ncbi.nlm.nih.gov/books/NBK500456/