The main symptom is a depressed mood that lasts most of the time. Depression should be distinguished from sadness, a natural emotion felt in situations of failure or loss. For example, a person who has lost a loved one and is experiencing considerable sadness while still undertaking normal activities can experience pleasure – they do not suffer from depression, but they experience mourning.
Depression – Symptoms and Types
Depression is a mental disorder. Its manifestations vary from patient to patient in terms of intensity and symptoms. It is crucial to accurately diagnose and customize treatment plans to meet the specific needs of each individual for the best possible outcome.
Symptoms of Depression
A depressive episode is a single period of at least two weeks during which symptoms such as:
- depressed mood for most of the day, regardless of external stimuli;
- sadness;
- lack of energy, increased fatigue, a feeling of constant tiredness;
- fatigue;
- loss of interest or pleasure in activities that used to give them pleasure (anhedonia);
- decrease in self-esteem and self-confidence;
- remorse and guilt;
- thoughts of death, suicide, suicidal tendencies;
- memory problems;
- difficulty concentrating, thinking, and making decisions;
- agitation (when accompanied by anxiety) or slowness of movement;
- sleep disorders – the most characteristic is waking up earlier than usual and not being able to fall asleep again; however, the diseases may have the form of difficulty falling asleep, frequent awakening or excessive drowsiness, and extending sleep up to several hours a day;
- eating disorders – decreased appetite and weight loss or increase, with weight gain;
- anxiety, a feeling of constant tension and worry;
- daily mood swings – a person suffering from depression usually feels the worst in the morning and in the evening notices some improvement;
- decrease in sex drive and in feeling pleasure.
When someone is sick, depression is not the only symptom that can affect their emotional state. If we suspect depression in a loved one, we should also pay attention to other symptoms like:
- a monotonous voice,
- slow body movements,
- frequent nervous changes in body position.
These signs may indicate anxiety, sadness, and poor facial expressions.

Not all sadness means depression, but if the symptoms persist for more than two weeks, it is a signal to seek help from a specialist who will conduct an interview, make a diagnosis, and suggest appropriate treatment.
Depression symptoms vary among individuals, which can cause misdiagnosis and improper treatment. Some individuals experience “masked depression” , where other symptoms are more prominent. Common signs of masked depression include sleep disturbances, anxiety, and physical symptoms like pain, breathing difficulties, or heart palpitations.
What Are the Severity Levels of Depression?
Depressive episodes can vary in severity. In mild and milder moderate cases, symptoms of depression may make it difficult, but not impossible, to perform duties and fulfill social roles. Sometimes, the functioning of such people seems correct, although they hide their ailments and suffering, and “being in good shape” can be an emotionally costly attitude. Severe depression, on the other hand, can make everyday activities practically impossible.
In severe episodes, sufferers may also experience:
- delusions – untrue, uncorrectable, and powerful beliefs, like about committing a crime, incurable disease, material ruin, death of one’s own or loved ones, catastrophe;
- hallucinations – false sensory perceptions, for example, voices encouraging to commit suicide;
- stupor – motor inhibition, interruption of contact with the environment.
Depressive episodes can occur singly, as the only episode in a person’s life. However, they are often recurrent or part of the picture of bipolar disorder, where apart from depressive symptoms, there are also manic, hypomanic, or mixed episodes.
Recurrent Depressive Disorders
Individuals who have endured two or more episodes of depression are diagnosed with recurrent depressive disorder, also known as unipolar depression or unipolar affective disorder. Over 50% of those who have already experienced a depressive episode will suffer a relapse, typically experiencing 3-5 episodes throughout their lifetime. Each relapse increases the risk of another recurrence and worsens the prognosis, reducing the chances of a complete recovery and increasing the likelihood of a chronic disorder course.
Causes of Depression
The causes of depression are complex and not fully understood. The following factors are believed to be necessary.
Biological factors are:
- genetic – the risk of depression is higher in families of people suffering from depression.
- Transmission disorders affect the brain’s chemicals, like serotonin, dopamine, and acetylcholine levels. Hormonal changes, particularly in stress hormones, have also been observed in people with depression.
- structural – the abnormal size of brain structures involved in regulating emotions has been observed in people suffering from depression.
- disorders in the inflammatory response – In depressive disorders, there are abnormalities in the secretion of factors that activate and inhibit the inflammatory response in the body. There is also an increased incidence of depression in diseases associated with this abnormality.
Certain psychological factors may increase one’s risk of developing depression. For instance, individuals with certain personality disorders may be more prone to depression, while those with high levels of anxiety as a personality trait may also be at higher risk. Additionally, people with better resources and coping mechanisms for dealing with stress are less likely to become ill. Finally, it has been observed that up to half of all first episodes of depression are preceded by adverse life events.
The most common social factors are lack of support, loneliness, and low social status.
Diagnosis of Depression
When diagnosing depression, a psychiatrist will conduct a thorough history-taking and mental state examination of the patient. It’s significant to gather information about coexisting mental disorders and illnesses that could increase the risk of depression or make treatment more difficult.
Additionally, it’s crucial to gather information about any drugs, dietary supplements, or stimulants the patient is using, as certain medications may intensify depressive symptoms while stimulants could lead to addiction as a complication of depression. For instance, alcohol abuse may temporarily “improve the mood,” but it worsens the patient’s condition because it is a depressant substance.
Helpful in diagnosis and monitoring Treatment progress can also be measured by symptom questionnaires(Beck’s Depression Inventory, Hamilton’s Depression Rating Scale, SHAPS – Snaith-Hamilton Pleasure Scale).
One of the elements of the diagnosis should also be screening for bipolar affective disorders (looking for symptoms of bipolar depression – like hypomanic symptoms).
Although it is not necessary to make a diagnosis, it may also be significant to plan laboratory tests that may indicate additional risk factors for depression – low levels of vitamin D, copper, zinc, folic acid, testosterone, or previously undiagnosed thyroid disease.

Comorbidity
Depression often co-occurs with other mental disorders and diseases like:
- mental disorders;
- anxiety disorders – very often accompany depression, and their coexistence is associated with worse prognosis and worse response to treatment;
- personality disorders;
- addictions and harmful use of psychoactive substances – may be the result of patients’ attempts to self-medicate with psychoactive substances, but depression can also be the result of both of these phenomena;
- eating disorders, in particular anorexia nervosa;
- sleep disorders (most often insomnia).
Other medical conditions that increase the risk of depression:
- chronic pain syndromes – more than half of patients suffering from chronic pain have symptoms of depression,
- neurodegenerative diseases (in particular Parkinson’s disease),
- malignant tumors,
- thyroid diseases,
- diabetes,
- stroke,
- heart attack – For patients who have had a heart attack, antidepressant treatment also reduces the risk of having another heart attack.
Treatment of Depression
Depression treatment usually happens in an outpatient facility, like a psychiatric or psychological clinic. However, if a patient has severe suicidal thoughts, tendencies, or psychotic episodes that put their life at risk, hospitalization is necessary. It’s crucial to work with the patient in developing a treatment plan and involve them in the process. To achieve this, psychoeducation is conducted to help the patient better understand their illness and treatment and to improve their cooperation during therapy.
Treatment of depression with currently available methods is usually effective – most patients experience remission of symptoms (like complete disappearance of symptoms of depression)
The main methods of treating depression are combinations of psychotherapy and pharmacotherapy. Check out why it is significant to combine those two methods.
Psychotherapy
The most effective form of psychotherapy for treating depression is cognitive-behavioral psychotherapy. However, other approaches, such as psychodynamic and interpersonal therapy, are also likely to be effective. Psychotherapy is just as effective as pharmacotherapy for mild to moderate episodes of depression. It can be used as the primary treatment for mild episodes.
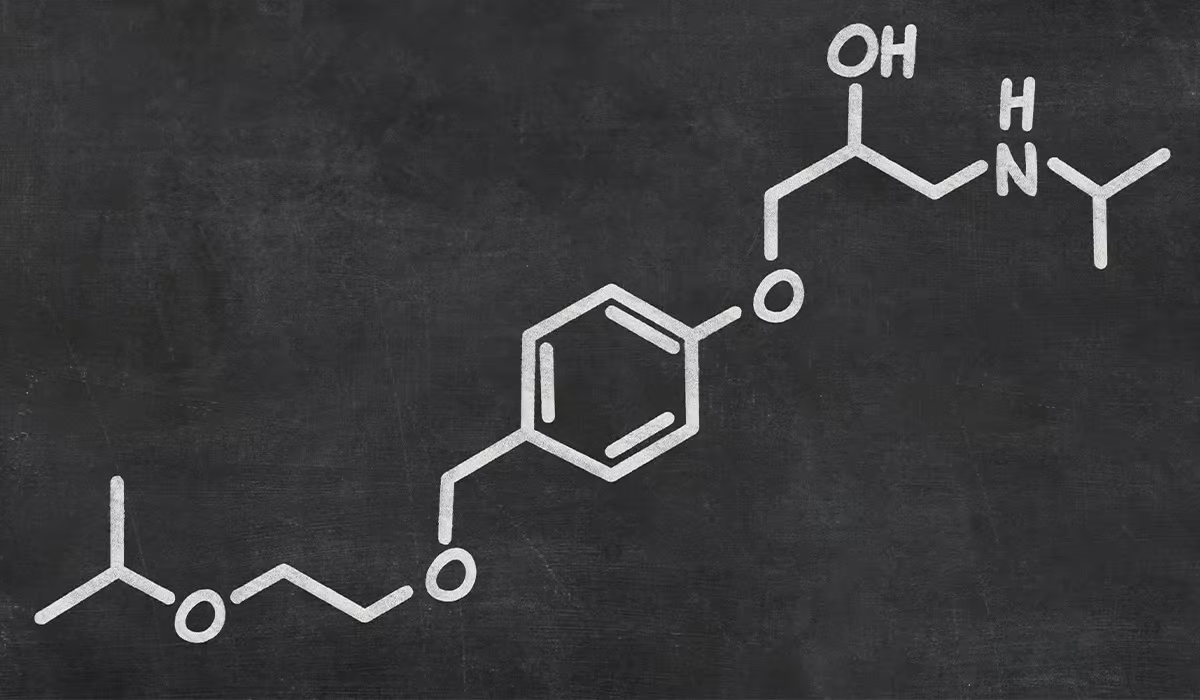
Pharmacotherapy – Drugs for Depression
Pharmacotherapy is currently the primary method of treating depression. Psychiatrists currently have a wide range of drugs for depression, which differ in their mechanisms of action (i.e., they have a specific effect on specific symptoms of depression) and side effects (for example, a soothing effect – it can be helpful to in agitated and anxious patients, and an activating effect – in sluggish patients, without energy).
Therefore, it is significant to discuss with the patient his expectations and concerns regarding pharmacotherapy so optimal drugs can be selected in the most individualized way. Modern antidepressants are effective and safe, but you should remember a few rules related to their use:
- antidepressants do not work right away (the therapeutic effect appears after approximately 2-4 weeks);
- medications should be taken daily, at fixed times, as recommended by a psychiatrist; they do not have a temporary effect, so do not modify the dose depending on your current mood;
- antidepressants are not addictive;
- taking antidepressants may be accompanied, especially in the initial weeks, by side effects; they are usually mild and transient (and are not an indication for discontinuation of the drug, and possibly for contacting the attending psychiatrist);
- treatment is long-term and should continue even after the symptoms subside, and its duration depends on how many episodes have occurred so far and how they proceeded;
- antidepressants should not be discontinued abruptly, as this is often associated with the risk of increased side effects.
It’s important to inform doctors from other specialties about taking antidepressants and to inform a psychiatrist about any drugs or dietary supplements being taken to avoid potential interactions.
During the pharmacotherapy of depression, observing possible drug-induced side effects is significant. As mentioned above, most of these symptoms go away independently, but some persist and can be troublesome. The psychiatrist discusses this with the patient during follow-up visits to modify the treatment if necessary. For example, changing a depression medication with a different mechanism of action is more beneficial for the patient.

It is important to note that antidepressants are not addictive. After they are discontinued too quickly, the so-called withdrawal symptoms but usually last several days and result from a sudden “lack” of drug molecules in the area of the relevant receptors.
If depression symptoms reappear after pharmacotherapy treatment, the illness hasn’t been cured, and continuing with pharmacotherapy is necessary.
Electroshock and Transcranial Magnetic Stimulation
Although it may evoke negative associations, electroconvulsive therapy is highly effective and safe for treating depression. Modern treatments involve a series of 10-12 sessions performed under general anesthesia. This treatment is recommended for conditions that require rapid improvement, such as depression with suicidal tendencies, increased psychotic symptoms, stupor, severe depression during pregnancy, and drug-resistant depression.
Transcranial magnetic stimulation is an alternative method to electroconvulsive therapy, which does not require anesthesia but, unfortunately does not have such high efficiency and speed of action.
Other Methods
In addition to traditional treatments, vagus nerve stimulation, deep brain stimulation, and neurosurgical techniques that target specific brain areas are sometimes used to treat depression. However, there is limited documentation on their effectiveness, and they are typically reserved for patients who have not responded to other treatments.
How to Support Loved Ones with Depression?
It’s important to understand that depression is a severe illness that cannot be quickly overcome. Avoid minimizing the patient’s feelings and struggles and try to empathize with them. Lack of support and understanding from loved ones can worsen the situation and lead to isolation.
Avoid saying:
- I can’t help you.
- I don’t understand you.
- Shouldn’t you feel better?
- Nothing happened! Stop complaining!
- It isn’t that bad. It could be worse.
- Get a grip.
- What’s wrong with you again?
- Try to think positively.
- It’s all in your head.
- Why are you behaving like that? You were always happy.
Instead use messages like:
- Tell me, how can I help you?
- Is something bothering you?
- You are not alone in this. You can count on me.
- I may not understand how you feel but remember that I am here for you and want to help.
- Your well-being will improve someday. Until then, you can count on me.
Prognosis
Although depression is an increasingly common disease, we have effective treatments, and the prognosis looks weel. The most important thing from the point of view of a person experiencing depressive symptoms and their relatives is not to underestimate these symptoms and seek help as soon as possible.
Treatment is usually safe. It may include pharmacotherapy or psychotherapy, and often, team care is indicated – provided by a psychiatrist and a psychotherapist. The latest generation drugs are not burdened with severe side effects, significantly facilitate everyday functioning, and help to derive measurable benefits from therapy.
Team treatment is currently the most effective method of helping patients and, depending on the severity of the disease, brings a relatively quick improvement in well-being.
Sources
- What Is Depression?. APA.
https://www.psychiatry.org/patients-families/depression/what-is-depression. - Depressive disorder (depression). WHO.
https://www.who.int/news-room/fact-sheets/detail/depression. - Depression. NIH.
https://www.nimh.nih.gov/health/topics/depression. - Causes – Clinical depression. NHS.
https://www.nhs.uk/mental-health/conditions/clinical-depression/causes/. - Overview – Antidepressants. NHS.
https://www.nhs.uk/mental-health/talking-therapies-medicine-treatments/medicines-and-psychiatry/antidepressants/overview/. - Prognosis of depression. Robert C. Baldwin.
https://journals.lww.com/co-psychiatry/Abstract/2000/01000/Prognosis_of_depression.14.aspx. - Depression in Adults with a Chronic Physical Health Problem: Treatment and Management. NIH.
https://journals.lww.com/co-psychiatry/Abstract/2000/01000/Prognosis_of_depression.14.aspx. - Understanding masked depression: A Clinical scenario. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5914271/. - Helping Someone with Depression. HepGuide.
https://www.helpguide.org/articles/depression/helping-someone-with-depression.htm. - Effects of Electroconvulsive Therapy on Depression and Its Potential Mechanism. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7044268/. - Transcranial magnetic stimulation as an alternative to electroshock therapy in treatment resistant depressions. A literature review. NIH.
https://pubmed.ncbi.nlm.nih.gov/9451566/. - Depression Assessment Instruments. APA.
https://www.apa.org/depression-guideline/assessment. - Comorbidity of Depression and Other Diseases. Masaru Mimura.