The characteristics most often used to characterize delirium are disturbances in consciousness and awareness. In the case of consciousness disorder, the patient feels disoriented both in time and space. However, attention disorders involve impairment of the concentration ability.
Delirium is not a mental illness. This condition is a set of symptoms that may appear during various somatic diseases. These symptoms most often appear after discontinuation of pharmaceuticals or psychoactive substances or in the occurrence of poisoning with them.

Causes
Consciousness disorders may be caused by one or more causes simultaneously. In many individuals, the delirium causes are multifactorial. The most common causes of consciousness disorders are:
- Immunological diseases
- Metabolic diseases
- Endocrine system diseases
- Vitamin deficiencies
- Anemia
- Porphyria
- Water and electrolyte metabolism disorders
- Acid-base balance disorders
- Neurological and neurodegenerative diseases
- Conditions leading to increased intracranial pressure
- Brain diseases
- Infarction dementia
- Alzheimer’s disease
- Strokes and head injuries
- Epileptic seizures
- Acute hydrocephalus
- Encephalitis
- Meningitis
- Carbon monoxide poisoning
- Systemic diseases
- Postoperative conditions
- Poisoning with psychotropic substances, sedatives, sleeping pills, and other psychoactive substances (e.g., a*********e, hallucinogens, cocaine, opiates)
- Alcohol abuse
- Circulatory system diseases
- Respiratory diseases
- Infectious and inflammatory diseases
- In older people, even minor infections
- Poisoning (e.g., carbon dioxide and monoxide, drugs, heavy metals, and industrial poisons: arsenic, lead, thallium, insecticides, volatile substances such as gasoline, organic solvents)
- Sudden discontinuation of medications (e.g., due to admission to hospital and failure to inform the doctor about the use of drugs)
The most important risk factors for delirium are:
- Age over 65 years
- Cognitive impairment and/or dementia
- Severe somatic disease
- Hypertension
- Fracture of the neck of the femur
- Stroke history
Symptoms
The most common symptoms of delirium include:
- Orientation as to time: the patient cannot provide the date, month, year, season, day of the week, place of stay (does not know where they are), and the situation they are in; these are the so-called allopsychic orientation disorders. Much less often, delirium involves a disturbance in self-orientation (i.e., auto psychic) – the patient does not know their name or who they are or gives false information.
- Logical thinking and attention (the patient’s statements are wholly or partially non-factual. They are characterized by varying degrees of impairment of accuracy and continuity; the patient has difficulty understanding questions asked by people around them; there is a marked weakening of vigilance, selectivity, and concentration of attention)
- Perception – visual hallucinations may occur, less often concerning other senses, e.g., auditory, tactile, and olfactory
- Emotions – the patient most often experiences fear, is anxious, and sometimes may react with aggression
- Psychomotor drive (from reduction, i.e., reduction of motor activity and the pace of mental processes to increased physical activity and motor and mental stimulation)
The course of consciousness disorders is characteristic, most often wavy and variable, with periods of improvement and deterioration. Symptoms most often worsen in the evening and at night. This variability in the severity of symptoms over the day differentiates delirium from dementia, in which the deterioration of cognitive functions is constant and slowly progressive. However, it should be remembered that people with dementia experience temporary disturbances of consciousness.
It happens quite often that transient disturbances of consciousness, especially those without arousal, go unnoticed and unrecognized. They may be missed when the patient only slightly slows down their speech rate and their statements contain vague, imprecise terms and inappropriate associations. Such patients seem helpless, confused and lost. This type of disorder may be a sign of a deterioration of the patient’s general condition or the first sign of an undiagnosed somatic disease.
Delirium is an acute disorder with sudden onset that may last from several hours to several hours to several days twelve days. However, it is sometimes preceded by prodromal symptoms, such as fear, anxiety, mood swings, insomnia, or nightmares. Their early diagnosis and appropriate treatment can significantly reduce the risk of developing full-blown delirium.
Diagnosis
Consciousness disorders can be diagnosed after:
- Mental health examination (assessing all the symptoms listed above)
- Examination of the patient’s physical condition (internal and neurological examination)
- Interview regarding the mental and somatic condition of the patient’s family members and/or medical staff (nurses, therapists, other staff) and analysis of data from medical documentation, including nursing reports
- Interview and tests for accompanying symptoms (fever, convulsions, headaches, disturbances in perception, thinking and speech, psychomotor drive, gait, in the performance of daily activities, appetite, bowel movements, urination, and sleep quality)
Special instruments are also used to assess cognitive functions during mental health diagnosis. These tests allow you to assess consciousness, deficits in cognitive processes, memory functions, disorders of coherence and train of thought, perceptiveness, orientation, and motor skills. The most well-known and commonly used tools are mainly used to assess the severity of dementia:
- A short examination of the mental state (Mini-Mental State Examination – MMSE), which allows for a superficial assessment of some cognitive functions, such as orientation in place and time, verbal memory, attention, language functions, and visuospatial analysis
- Clock drawing test (CDT), allowing for the assessment of visuospatial processes, construction skills, and abstract thinking through qualitative analysis of the results

There are also several helpful instruments for assessing only disturbances of consciousness. The most uncomplicated tools include the Confusion Assessment Method (CAM), which is a short screening tool. It can be used by doctors, including those who are not psychiatrists, to diagnose consciousness disorders in patients from somatic wards, as well as in surgical patients. The test consists of 4 items, and the finding of symptoms from items 1 and 2 and one of the symptoms from item 3 or 4 confirms the presence of consciousness disorders:
- Sudden changes in mental status that change over minutes or hours
- Attention disorders (e.g., difficulties in counting and listing the days of the week backward)
- Quantitative disturbances of consciousness (e.g., fogginess and drowsiness)
- Thought disorders (e.g., incoherent statements)
In a patient with suspected or diagnosed consciousness disorders, the basic functions of the circulatory system (blood pressure, heart rate, and ECG) and respiratory system should be monitored. Mandatory laboratory tests include a complete blood count with smear and erythrocyte sedimentation rate, arterial blood oxygen saturation, electrolyte and glucose levels, liver enzyme activity, albumin, creatinine, urea, and acute phase protein levels, and a urine test.
When assessing unclear causes of delirium, the specialists may recommend doing additional examinations, including:
- Computed tomography or magnetic resonance imaging of the head
- X-ray of the lungs
- Brain electroencephalography (EEG)
- Cerebrospinal fluid tests
- Blood tests
- Urine tests for the content of toxic substances and drugs and urine culture
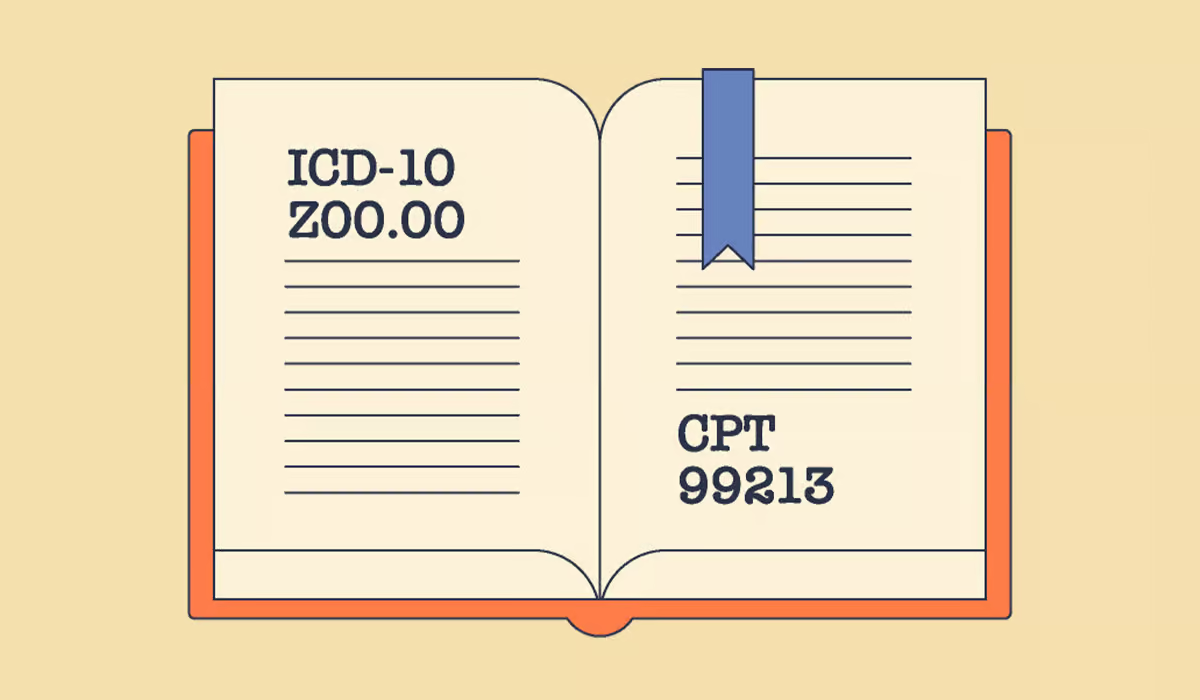
ICD-10 Diagnostic Criteria for Delirium
The specialists may also use the International Statistical Classification of Diseases and Related Health Problems (ICD) to make a firm diagnosis of delirium. According to ICD-10, symptoms should be present in each of the following areas:
- Impairment of consciousness and attention (ranging from drowsiness to coma, reduced ability to direct, focus, sustain, and shift attention)
- General cognitive disturbances (perceptual distortions, illusions, and hallucinations – most often visual; impairment of abstract thinking and understanding. Presence or absence of transient delusions (usually with some degree of incoherence); disturbances in immediate memory, but with relatively intact distant memory; confusion about time and, in more severe cases, about place and people
- Psychomotor disturbances (hypo- or hyperactive and unpredictable changes, prolonged reaction time, increased or decreased fluency in speech, increased reaction)
- Disruption of the sleep-wake cycle (insomnia or, in severe cases, complete loss of sleep or reversal of the sleep-wake cycle, daytime sleepiness, worsening of symptoms at night, disturbing dreams or nightmares which may be hallucinations upon awakening)
- Emotional disorders include depression, anxiety or fear, irritability, euphoria, apathy, or confusion. The onset is usually rapid, the course of delirium varies throughout the day, and the total duration of the condition is less than six months
The above clinical picture is so characteristic that a confident diagnosis of delirium can be made quite quickly. It happens even if the specialist cannot clearly define the underlying cause. In addition to the underlying disease, these symptoms provide evidence of the presence of brain dysfunction (e.g., usually an abnormal electroencephalogram, but not always). If activity slows, additional tests may be necessary if the diagnosis is in doubt.
Treatment
Treating delirium is difficult and usually requires at least several days for stabilization. The most essential thing is to remove the possible reasons (e.g., blood oxygenation disorders, increased/lowered blood sugar levels, fever). Additionally, psychotherapy and direct coercion or immobilization are used if a person suffering from delirium poses a threat to themselves or others.
Many specialists recommend pharmacotherapy. Commonly used tranquilizers may enhance consciousness disorders, and sedative benzodiazepines should only be used in patients with alcohol-related delirium because, in classic delirium, they may permanently impair cognitive functions.
In exceptional circumstances (e.g., intensive care), temporary sedation using some medicaments is permissible. However, any prolonged sedation may increase consciousness disorders and cause permanent neurological deficits.

According to the proverb “prevention is better than cure,” it is worth using delirium prevention, which includes:
- Regular monitoring of patient parameters (saturation, pressure, hydration, blood sugar level)
- Regular assessment of the state of consciousness
- The presence of a 24-hour clock in the sick person’s environment
- The presence of close relatives with the sick person
- Ensuring that the sick person always has glasses and a hearing aid
- Early removal of catheters and cannulae
- Early getting the sick person out of bed
- Regular irrigation
- Taking care of regular bowel movements and kidney function
- Ensuring the good quality of sleep of a sick person
How to Help an Individual with Delirium?
A person suffering from delirium may behave irrationally and pose a threat to themselves or those around them. Therefore, when symptoms of delirium occur, they should be provided with constant care, and appropriate conditions in the room where they stay should be ensured. It is worth setting the clock in a visible place and opening the windows to make the patient more aware of the time.
You should also converse with them as much as possible so that they don’t forget where they are and who the individuals around them are. It is also necessary to ensure the patient has enough fluids because dehydration is an additional factor exacerbating delirium. In case of aggressive behavior, the caregiver should not raise their voice but slowly and clearly explain to the patient what their condition is and constantly calm them down.
In circumstances where delirium cannot be prevented, supporting the suffering person is most necessary. They may be disconnected and scared; they don’t know where or what is happening. Good support for a person in delirium will be:
- The presence of a loved one during the duration of the disorder
- Bringing the sick person something familiar from home (e.g., a framed photo of the family)
- Writing down in a diary what happened to the person during the period of delirium
- Reducing noise and lighting
- Providing the sick person with maximum peace
- Speaking to a person in delirium in short and understandable sentences
- Calling a person in delirium by name
- Not responding with aggression to the potential aggression of a sick person – a person in delirium does not realize what they are doing and does not understand why they are being shouted at
Sources
- Delirium. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK470399/. - Sudden confusion (delirium). NHS.
https://www.nhs.uk/conditions/confusion/. - The major risk factors for delirium in a clinical setting. NIH.
https://pubmed.ncbi.nlm.nih.gov/27499625/. - Overview. NHS.
https://www.guysandstthomas.nhs.uk/health-information/delirium-sudden-confusion. - Delirium in elderly adults: diagnosis, prevention and treatment. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3065676/. - The Mini-Mental State Examination as a diagnostic and screening test for delirium: systematic review and meta-analysis. NIH.
https://pubmed.ncbi.nlm.nih.gov/25267696/. - A systematic review and meta-analysis of the accuracy of the clock drawing test (CDT) in the identification of delirium in older hospitalised patients. NIH.
https://pubmed.ncbi.nlm.nih.gov/32091236/. - Confusion Assessment Method for the intensive care unit (CAM‐ICU) for the diagnosis of delirium in adults in critical care settings. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6513664/. - 2024 ICD-10-CM Diagnosis Code R41.0. ICD-10.
https://www.icd10data.com/ICD10CM/Codes/R00-R99/R40-R46/R41-/R41.0. - Clinical Practice Guidelines for Management of Delirium in Elderly. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5840908/. - Pharmacologic treatment of delirium symptoms: A systematic review. NIH.
https://pubmed.ncbi.nlm.nih.gov/36375344/. - Delirium: prevention, diagnosis and management in hospital and long-term care. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK553009/.