Sick people can consume up to several thousand calories in a short amount of time. Such an episode is followed by shame, associated with the need to “get rid” of the eaten food and lose weight. Such compulsive eating and then purging cycles may occur several times a week.
Bulimia is an eating disorder – a disease associated with experiencing severe, health-threatening eating behaviors and related emotions and thoughts.
Bulimia causes the everyday life of sick people to focus on eating, self-control, and body weight control. This established pattern is interrupted by periodically occurring, uncontrolled attacks of the so-called gluttony, after which the patient undertakes several activities to “counteract the effects” of excessive amounts of food.
Types
Bulimia nervosa is a heterogeneous disorder in terms of its clinical picture.
Depending on the behavior that occurs after an episode of compulsive overeating, there are two basic types of bulimia:
- Purging type – after an attack of gluttony, a bulimic wants to expel the consumed content as quickly as possible. They induce vomiting, take laxatives and enemas, and also take diuretics that stimulate the kidneys and stimulate the excretion of water from the body.
- Non-purgative type – compensation occurs without vomiting and diarrhea, but the means to achieve the goal is a strict diet, sometimes even a multi-day fast. Sometimes the patient prescribes backbreaking physical exercises, pushing their body to the limits of its capacity.
This typology, although very general, perfectly shows how dangerous a disease advanced bulimia is. It is not difficult to guess that the practices described quickly lead to the accumulation of emotional problems and the physical degradation of the body.
Causes
The causes of bulimia include biological, individual, and family factors.
Biological factors of bulimia include, among others, abnormalities in the functioning of the serotonergic system and interactions between substances such as leptin or dopamine, which affect appetite.
Individual characteristics include difficulties with self-acceptance or low self-esteem. People suffering from bulimia usually do not like themselves, they disregard themselves, and they mistreat themselves. They base their opinions about themselves on the views of other people who are significant to them. These may be parents, siblings, or partners. It is mainly their opinion that determines what the patient will think about themself.
Moreover, people with bulimia strive for acceptance of their surroundings even at the cost of giving up their needs, which usually confuses low well-being and tension. A lack of success may also cause the latter because patients are often very ambitious. They also need to be controlled.
Family factors include hostility in the home and lack of support, warmth, or models for effectively dealing with conflicts. Another factor may also be obesity in the family or a crisis related to the home environment, divorce, or the death of a loved one. Stressful situations such as exam stress, job change, and even pregnancy may also play a role in the pathomechanism of the disease.
Symptoms
Bulimia nervosa is characterized by the following symptoms:
- Problems with teeth and gums, including caries and various types of inflammation, are often the first tangible symptom of the disease. It happens due to the action of stomach acids, which, together with induced vomiting, enter the oral cavity in large quantities. This symptom is visible after about six months. Additionally, the cause of dental caries may be the consumption of large amounts of sugar during binges and hygiene negligence, which is typical of this phase. The final consequence may be tooth loss or the need to extract them.
- A dry mouth results from reduced salivation, which is related, among other things, to general body dehydration.
- Dry skin and hair are another consequence of dehydration.
- Heartburn, i.e., burning sensation in the esophagus and even vomiting blood, is related to the action of stomach acids on the delicate mucous membranes of the upper parts of the digestive tract.
- Cardiac disorders are associated with the loss of large amounts of electrolytes, such as potassium, which occur as a result of vomiting and the use of laxatives.
- Fatigue, lethargy, irritability, anxiety, as well as depression and anxiety, feelings of shame and self-loathing, and other mental symptoms.
- Loss of natural intestinal peristalsis, resulting from its frequent stimulation with drugs and other preparations that accelerate defecation. After stopping their use, constipation and abdominal pain may occur, which encourages many people to return to their old practices, creating a vicious circle.
- The hamster’s face is a swelling visible on the cheeks, which is a manifestation of inflammation of the salivary glands.
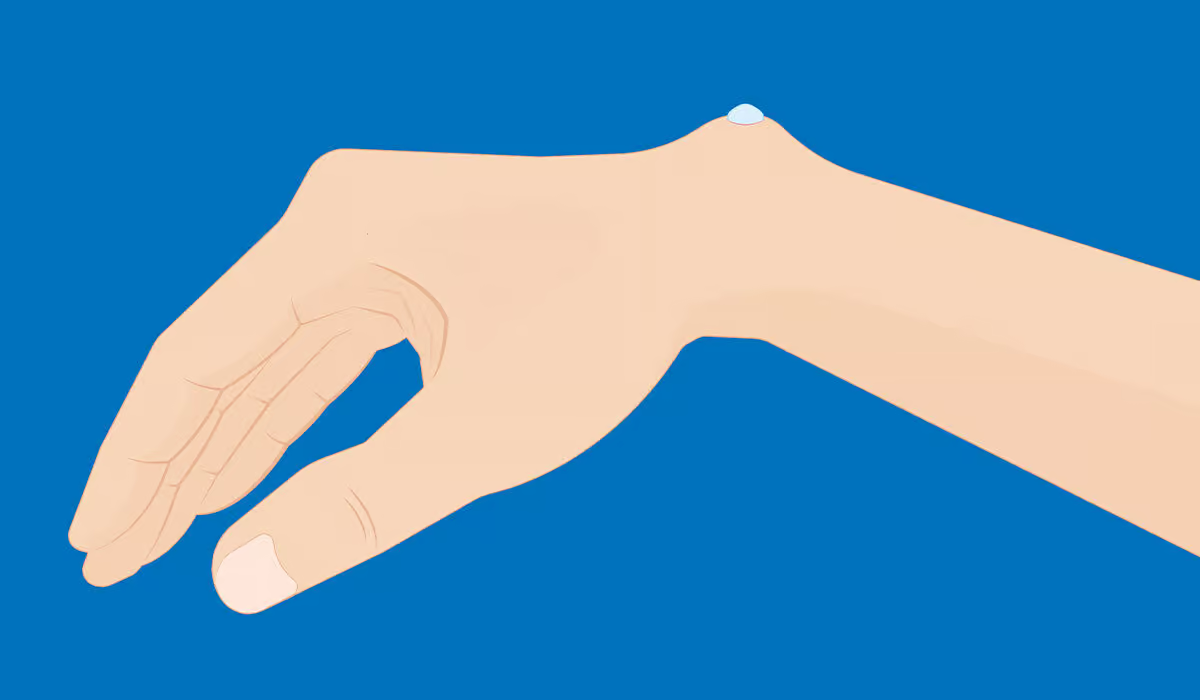
- Russell’s sign is the appearance of scars on the fingers of the hands, associated with inducing vomiting by putting the hand into the mouth (damage is a consequence of rubbing against the teeth, especially the sharply pointed incisors).
- Menstrual disorders and possible difficulties in getting pregnant due to lower concentration of the so-called luteinizing hormone.
- As already mentioned above, many people ask whether bulimia causes weight loss. The answer may seem surprising. Unlike anorexia, which involves significant weight loss, bulimics usually neither gain nor lose weight.
This is related to developing a pathological but effective mechanism for balancing the amount of food consumed and compensating for gluttony through vomiting, diet, or training.

Diagnosis
The diagnosis is made by an internist, psychiatrist, or psychologist based on an interview and appropriate tests.
During the interview, the following is checked, among others:
- Whether there are repeated episodes of binge eating
- Whether vomiting is induced or laxatives are used
- Whether fasting or intense physical exercise is used
- How often and how long, if any, binge eating episodes occur
- What is an indicator of self-esteem
After an interview and tests, if the diagnosis is bulimia nervosa, appropriate treatment is proposed and implemented.
The diagnostic criteria for bulimia nervosa are included in the international classification of diseases of the WHO (ICD-10) and the American Psychiatric Association (DSM-5).
The diagnostic process, according to ICD-10 includes:
- Recurrent episodes of binge eating (at least twice a week for three months), during which large amounts of food are eaten in a short period
- The patient attempts to counteract the effects of “weight gain” by one or more of the following methods: inducing vomiting, provoking stool excretion, subsequent periods of starvation, and/or use of appetite suppressants, thyroid preparations, and diuretics; in the case of bulimia in diabetics, patients can downplay insulin treatment
- Self-esteem as an obese person and disturbing fear of gaining weight (usually leading to underweight)
The diagnostic process according to DSM-5 includes binge-eating episodes characterized by eating amounts of food in a short period that are much larger than what most people would eat in a similar time and under similar circumstances (e.g., 2-3 hours), and feeling a loss of control over eating during an episode. Moreover, there are:
- Repetition of compensatory behaviors aimed at preventing weight gain (including inducing vomiting, inappropriate/excessive use of laxatives, diuretics, or other substances, fasting, and excessive physical exercise)
- Episodes of overeating and inappropriate compensatory behaviors occur on average at least once a week for three months
- The patient’s self-esteem depends on the subjective assessment of figure and body weight
- The disorder does not occur exclusively during episodes of anorexia nervosa
Treatment
Treatment often takes a long time, even years. It is necessary to repair the relationship with food, regulate meals, and provide the right amount of nutrients in the diet, which will help prevent attacks of ravenous hunger. The treatment process usually involves a psychotherapist (specialists recommend cognitive-behavioral psychotherapy as the first-choice therapy) and a dietitian.
People with eating disorders should not be referred to specialists in the field of nutrition or dietetics who do not have knowledge and experience in the field of nutritional psychology and psycho-dietetics.

The standard in psychiatric pharmacological treatment of bulimia is the use of drugs classified as so-called serotonin reuptake inhibitors (SSRIs). These substances inhibit the capture of the hormone serotonin by neurons, thereby increasing its level in the brain. They are used primarily to treat depression, but they are also used for other ailments. Patients often ask about appetite suppressants. In the case of bulimia, which is a mental illness, such measures are not part of the standard of care.
It is also necessary that the above-mentioned drugs for bulimia cannot be purchased without a prescription. These are psychotropic substances that are generally available in pharmacies only with a doctor’s prescription.
Sometimes, a doctor’s involvement (even a psychiatrist) must also be necessary. If the patient’s body weight is incorrect, then only in the background (after regaining control and repairing the relationship with food) is the possible weight loss (if the body weight is too low, it usually returns to normal earlier when a rational diet is introduced).
Bulimia nervosa is usually treated on an outpatient basis. A hospital stay is rarely necessary unless very severe symptoms of depression coexist, and this is the only solution to ensure the patient’s safety.
Consequences
Untreated bulimia, especially if it lasts for many years, has severe consequences for the health of the entire body. One of the first symptoms is progressive caries. This problem results from daily vomiting, which causes gastric juices to leak into the mouth and damage tooth enamel.
Frequent vomiting and the use of laxatives can cause electrolyte disturbances. Losing potassium, sodium, and chlorine causes muscle weakness, uncontrolled cramps, and headaches.
A decrease in potassium concentration may lead to metabolic alkalosis, which manifests itself in impaired consciousness, memory, and concentration, anxiety attacks, dizziness, heart rhythm disturbances, drop in blood pressure, respiratory muscle dysfunction, and muscle spasms of the entire body. Patients with metabolic alkalosis who stop the dangerous practices of purging and vomiting experience weight gain.
Although it is only caused by water retention in the body tissues, it often encourages people suffering from bulimia to continue losing weight in their current way, which is dangerous to their health and life.
Binge eating can also cause acute pancreatitis. Bulimia may also cause rupture of the stomach or esophagus.
Other possible complications from the digestive system include inflammation and ulceration of the esophagus, vomiting blood, enlargement of the submandibular glands, persistent constipation, intestinal atony, bloody diarrhea, and rectal prolapse. Constipation and delayed gastric emptying occur as a result of slower intestinal peristalsis. Provoked vomiting in bulimia may cause aspiration pneumonia – gastric acid escaping from the stomach during vomiting may reach the lungs, causing infections and inflammation, which may be dangerous to health.
In bulimia, the hematopoietic function of the bone marrow may also be impaired, which in turn leads to anemia and thrombocytopenia. Cardiac complications may include accumulation of fluid in the pericardium and damage to the valves and heart muscle.
In extreme cases, brain tissue trophies, and the peroneal nerve becomes paralyzed – then the footfalls and it cannot be lifted while walking. Women with too low body weight and stopped menstruation are at increased risk of osteoporosis. Another common complication affecting women is ovarian cysts and infertility caused by anovulatory cycles.
More severe complications are observed in patients with bulimia, who are debilitated by the use of dangerous methods of weight loss, such as pharmacological purging, induction of the vomiting reflex, and taking large amounts of diuretics and synthetic thyroid hormones.
The consequences of untreated bulimia are not only physical. In the mental sphere, bulimia leads to numerous disorders such as remorse, low mood, low self-esteem, and self-blame.
Prevention
Prevention of bulimia and other eating disorders is challenging. Eating disorders do not have a clear, clearly noticeable beginning. As a rule, it is difficult to identify the causative agent before the disease occurs and before the patient undergoes therapy.
What is significant bulimia nervosa most often affects young people who are already mature or sexually mature but still mentally immature and do not have considerable life experience. That is why the role of parents or guardians and teachers is so important, and they should react to any dangerous signs of the disease.
What you need to pay attention to are:
- Eating irregularities, with a clear division into phases of gluttony and fasting
- The child’s frequent vomiting or defecation, the presence of laxatives in his room, visible scratches on his hands, or his teeth decaying quickly
- Excessive focus on appearance, with particular emphasis on weight and circumference, critical assessment of one’s figure, and frequent reference to “ideals” from the Internet or television
What a parent can do to help their child early is undoubtedly a conversation – honest but delicate, respecting the intimate areas of the teenager’s emotionality.
If you suspect something, consult an eating disorder specialist and establish an action plan together. Everything should be done to ensure that the child begins treatment as soon as possible, but too sudden and forceful actions in this matter may have the opposite effect.
It is also worth putting great emphasis on family relationships daily. Various studies show that disturbed parent-child relationships may also be a significant contributor to the development of bulimia.
Sources
- Bulimia Nervosa. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK562178/. - Classification of bulimic-type eating disorders: from DSM-IV to DSM-5. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4081768/. - Overview – Bulimia. NHS.
https://www.nhs.uk/mental-health/conditions/bulimia/overview/. - Symptoms – Bulimia. NHS.
https://www.nhs.uk/mental-health/conditions/bulimia/symptoms/. - The Diagnosis and Treatment of Eating Disorders. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3221424/. - 2024 ICD-10-CM Diagnosis Code F50.2. ICD 10.
https://www.icd10data.com/ICD10CM/Codes/F01-F99/F50-F59/F50-/F50.2. - DSM-IV to DSM-5 Bulimia Nervosa Comparison. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK519712/table/ch3.t16/. - Bulimia nervosa in adolescents: prevalence and treatment challenges. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5757497/. - Bulimia nervosa. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3275326/. - Health Consequences of Eating Disorders. NEDA.
https://www.chapman.edu/students/health-and-safety/psychological-counseling/_files/eating-disorder-files/4-hlth-cons.pdf. - Eating Disorder Prevention: Current Evidence-Base and Future Directions. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3926692/.