There is no need for supplementation as breast milk provides nourishment and hydration. The World Health Organization does not specify the duration of breastfeeding; it should be based on the unique needs of the mother and the baby.
What Is Lactation?
Lactation is a physiological process related to the production and secretion of milk in a woman’s mammary glands. This process begins during pregnancy and fully develops right after the baby’s birth.
In the first two hours after giving birth, medical staff encourage the new mother to breastfeed because it is the best way to provide the baby with the nutrients necessary for proper development.
Hormones
The hormone prolactin regulates the portion of milk a woman produces, and the organism starts creating prolactin earlier in pregnancy. Primarily, the high concentration of estrogen, progesterone, and other hormones stop prolactin. Those pregnancy hormones decrease once the placenta is delivered, and prolactin takes control.
When the baby suckles, it stimulates nerves that notify the organism to release prolactin and oxytocin. Prolactin induces the alveoli to produce milk, and oxytocin induces muscle contractions that move out of the alveoli and through the milk ducts.
When milk is released, it takes about 30 seconds of suckling before the letdown happens. Because a woman can not control which breast acquires the hormones, the letdown may induce milk to leak from both nipples.
Generating lactation in non-pregnant individuals demands medication that simulates hormones the organism produces during pregnancy. Suckling from the nipple may provoke lactation, either with a breast pump or by a baby. It is a complicated procedure that requires working closely with a healthcare provider who comprehends the requirements of non-pregnant individuals and has knowledge of initiating lactation.
How To Stimulate Lactation?
Many breastfeeding women have trouble maintaining lactation at a satisfactory level. If your breasts do not produce enough milk, following the tips below is worth it. The most important thing is to put the baby to the breast frequently, as well as at night because that’s when the prolactin level is the highest. It is also important to give your baby both breasts while feeding, not just the favorite one. Regular sucking and emptying of the breast stimulates the secretion of prolactin, thus increasing milk production.
Other helpful methods include:
- Correct feeding technique (incorrect feeding technique makes it difficult to empty the breasts effectively)
- Maintaining closeness to the child, frequent skin-to-skin contact
- Maintaining a balanced diet and proper hydration of the body
- Positive attitude, limiting exposure to stress
- Drinking fennel tea
- Using dietary supplements that stimulate milk production (preferably after consulting a doctor or midwife)
Lactation problems can effectively discourage breastfeeding, which harms both mother and baby. If none of the above methods bring improvement, it is worth consulting a lactation consultant.
Advantages
Breastfeeding helps to give a baby the nutritious food needed to grow healthy. However, that is not the only advantage.
For The Child
Breastfed infants, compared to those fed with formula, have lower chances of being hospitalized, whether in developed or developing countries. This happens because they are better protected against respiratory, digestive, and middle ear infections. They also have reduced risks of urinary tract infections, bacterial meningitis, and fever following vaccinations. Moreover, SIDS is three times less common among breastfed infants.
Exclusively breastfed children, especially in the first months of life, obtain greater health benefits later in life than children fed with formula or supplemented with it. They have a lower risk of being overweight, having obesity, type 1 and type 2 diabetes, cancer (leukemia, malignant lymphoma), asthma, atopic dermatitis, and nutritional deficiencies. Adults whose mothers breastfed are much less likely to have problems with increased cholesterol levels, atherosclerosis, hypertension, and ischemic heart disease.
Breast milk is the safest nutritional substance for prematurely born children, ensuring proper development and protecting against necrotizing enterocolitis (NEC), sepsis, and other disorders of the immature body.
Exclusively breastfed children for the first 6 months of life grow and develop normally. Breastfed children experience better cognitive function development and have better psychomotor development indicators.

For A Breastfeeding Mother
Breastfeeding not only benefits the baby but also the mother in various ways:
- It creates a strong bond with the child
- The mother experiences reduced discomfort during the first 6 weeks after giving birth, with her uterus shrinking faster, shorter postpartum bleeding, and a lower risk of anemia
- It helps the mother lose the extra weight gained during pregnancy more quickly
- There is a lower risk of overweight and obesity
- There is a reduced risk of postpartum depression and later-life depression
- The mother has a lower likelihood of developing breast and ovarian cancer, especially with longer durations of breastfeeding
- There is a decreased risk of hip fractures and osteoporosis in old age
- Breastfeeding for more than 12 months decreases the likelihood of hypertension, diabetes, hyperlipidemia, and ischemic heart disease in the postmenopausal period
Social Benefits
Feeding is cheap. Its cost comes down to the mother’s nutrition and possibly feeding accessories. If more complex problems arise, you may need the help of a lactation consultant, who is usually paid. If lactation is going well, accessories are also unnecessary for a short time. These expenses are much lower than the price of artificial feeding. In this case, we have fixed costs related to the purchase of mixtures and accessories but also hidden costs – related to increased morbidity. The costs of treating sick children and then adults are significant, as they include medicines and doctor’s work, commuting, time off work, hospital treatment, pensions, and rehabilitation.
Feeding is ecological – it does not produce waste or greenhouse gases. The production of artificial mixtures is expensive and involves breeding cows, the work of food technologists and chemists, laboratory and factory work, packaging production, waste disposal, etc.
Feeding is practical and comfortable. The food does not need to be prepared, sterilized, heated, poured into bottles, etc. It is always ready at any time, at home or while traveling. This convenience means that a breastfeeding mother can fully enjoy her life. For this purpose, she does not have to be separated from her child or the rest of the family.
The Most Common Lactation Problems
Breastfeeding presents a range of experiences for women, from profoundly rewarding to challenging and painful. Idealized portrayals of breastfeeding in media and advertising often diverge from the reality experienced by many women. Lactation problems, which significantly impact the health and well-being of both the breastfeeding woman and her child, receive limited attention in public discourse.
The most common lactation problems include irritated nipples, with the potential for bacterial infection, mycosis of warts, flat or inverted nipples, allergic skin changes such as erythema and excessive exfoliation, breast inflammation, food deficiency, and lactation crisis.
Mother’s milk is a meticulously balanced source of nourishment for the infant, providing comprehensive nutrition essential for proper development. Despite their optimal composition, alternate milk formulations cannot rival the benefits offered by nature’s provision.
Health Problems
Although breastfeeding has many advantages, in some cases, people try to avoid it. Mostly, that is because women have a medical issue. One of them is a common cold.
Cold And Breastfeeding
What should a breastfeeding woman do when she has a cold? Some initial thoughts are to stop breastfeeding to protect the baby from getting sick. Is that the right thing to do?
The World Health Organization recommends breastfeeding babies until they are six months old due to its numerous health, developmental, psychological, and social benefits. Even after introducing solid foods, breastfeeding should be continued for at least two years.
There are very few reasons that would require stopping breastfeeding, such as HIV, early tuberculosis, maternal drug addiction, or galactosemia in the child. There are also temporary reasons and some debatable cases, like alcoholism, viral liver infections, or mastitis.
Can You Breastfeed During A Cold?
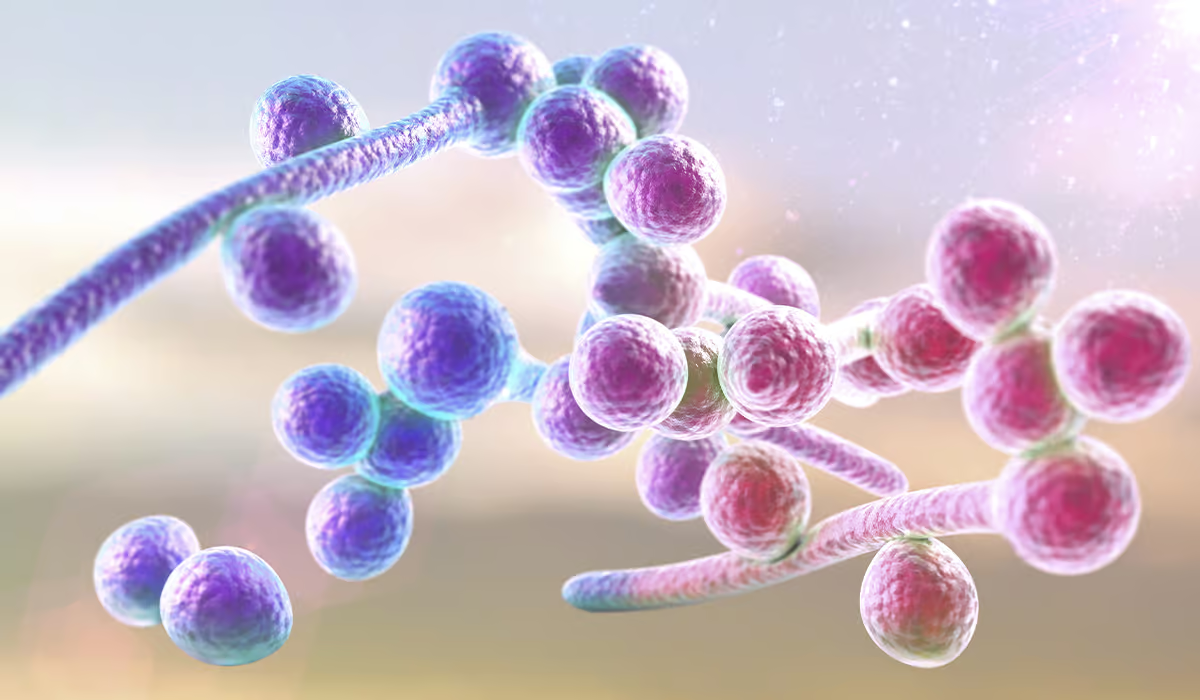
Yes, you can breastfeed during a cold, and it’s recommended. When you have a cold, the antibodies your organism produces can pass to your baby through breast milk, giving them extra protection. This helps them build immunity against the virus. If a baby is not breastfed or is temporarily weaned, they won’t benefit from this immunity. So, breastfeeding during a cold is beneficial for your baby.
Now, in addition to discussing breastfeeding during a cold, it’s essential to address how to treat a cold while breastfeeding.
What To Treat A Cold While Breastfeeding?
The best treatment for a cold while breastfeeding depends not only on the effectiveness of various remedies from the point of view of a sick, breastfeeding mother. What also counts, and perhaps above all, is the child’s safety. Can you take medications during this time, and if so, which ones?
Although information on this subject is available, remember to consult a doctor before using any medicine, who will advise or recommend what you can take for a cold, including prescription and over-the-counter medicaments.
What Are The Breastfeeding Positions?
A woman needs to adopt the proper position for feeding the baby, which will be comfortable for both the mother and her baby.
It is not only when the mother gives the baby food but also when you can build a bond between the parent and the baby. This natural closeness can have a positive impact on the child’s development.
Each of the feeding positions discussed below should be comfortable for both parties. The mother can lie or sit and must use her hands and arms to support the baby’s head and back. You can use support under your knees and feet and a pillow under your back to further increase comfort during this activity.
The correct feeding position requires proper posture – the baby’s head, shoulders, and torso must be in one line. The baby’s face should be turned towards the breast without turning the neck. You need to ensure that the baby’s body fully adheres to the mother’s body, but the baby must also be able to tilt the breast away from the head.

Examples
Now, you can choose one of the breastfeeding positions. Here are some suggestions:
- The classic position is when the baby cuddles its tummy to its mother’s belly. The baby’s head rests on the mother’s shoulder, and her hand supports the buttocks. The other hand gives the baby the breast
- Armpit position – also called football position, which involves positioning the baby in such a way that its legs are under the mother’s armpit
- Cross position – when the baby’s head is held by the hand of the side opposite to the side of the breast that the mother is feeding, e.g., right hand – left breast
- Side-lying position – in this position, the mother lies sideways and pulls the baby towards herself
- Lying on the back position – the mother can lie on her back and the baby is placed along the body or diagonally
The position in which to feed a newborn or an older child depends on you but also on your health condition. Some positions will work better, e.g., after a cesarean section.
Other Important Factors
It is also significant that the baby grasps the nipple correctly. The toddler has captured it properly, as evidenced by, among other things, the fact that the baby’s upper and lower lips, when opened, form a wide angle and the baby’s nose and chin touch the nipple.
Moreover, you should check whether your baby has grasped the entire nipple and most of its areola and whether their cheeks are filled. After a successful feeding, the nipple is not flattened. This is one of the indicators that everything turned out well.
Breastfeeding can’t hurt. If you feel pain, it’s a sign that something is wrong. You can then put a clean finger into the baby’s mouth and interrupt the feeding to improve the position.
Sources
- Physiology, Lactation. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK499981/ - Breastfeeding. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK534767/ - Benefits of breastfeeding. NHS.
https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding/benefits/ - Breastfeeding-Related Health Benefits in Children and Mothers: Vital Organs Perspective. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC10536202/ - Common breastfeeding problems. NHS.
https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding-problems/common-problems/ - Breastfeeding and complementary feeding. WHO.
https://www.paho.org/en/topics/breastfeeding-and-complementary-feeding - Breastfeeding and medicines. NHS.
https://www.nhs.uk/conditions/baby/breastfeeding-and-bottle-feeding/breastfeeding-and-lifestyle/medicines/ - Breastfeeding positions. NHS.
https://www.nhs.uk/start-for-life/baby/feeding-your-baby/breastfeeding/how-to-breastfeed/breastfeeding-positions/