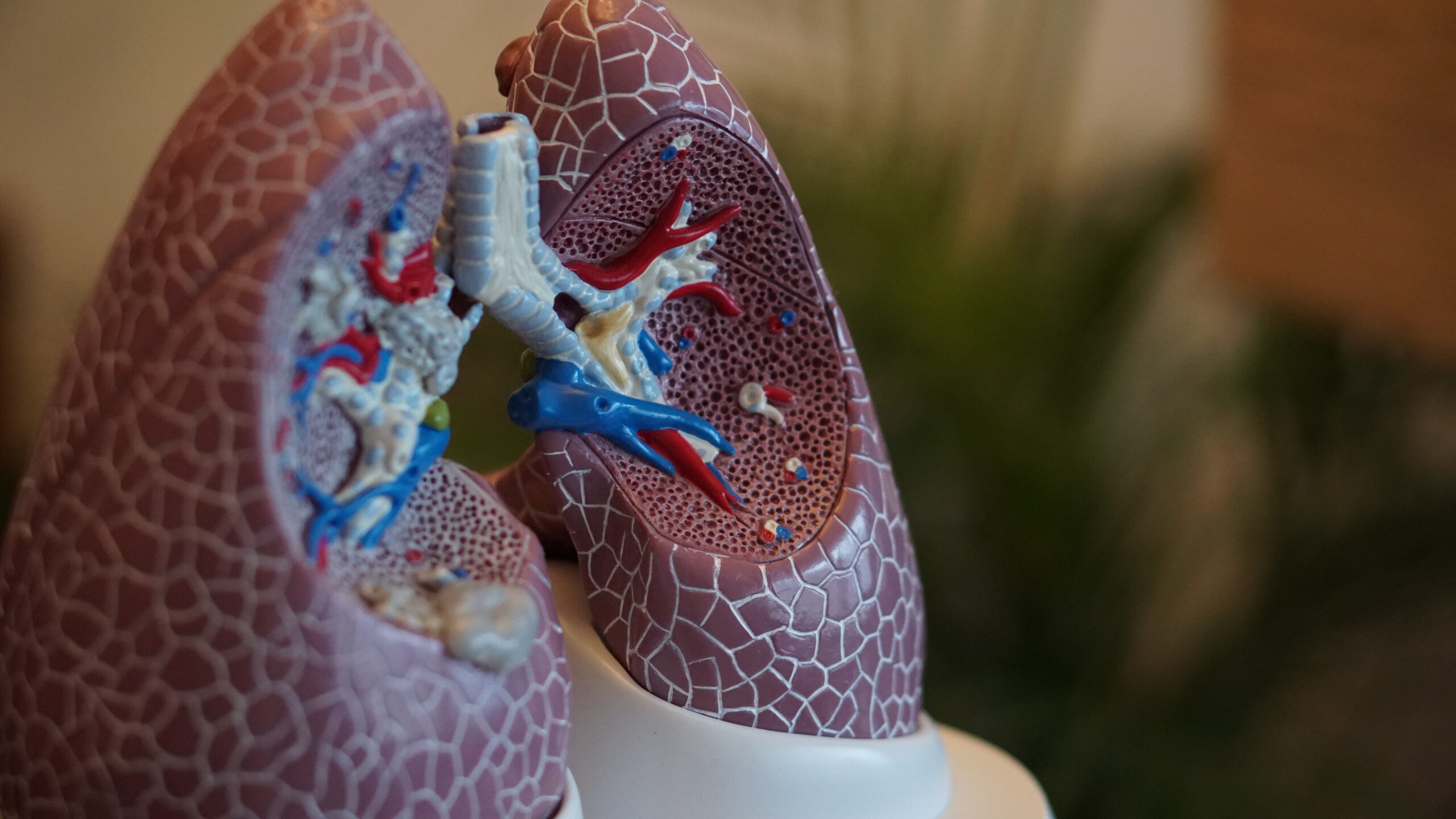
To breathe in and out correctly, lungs must have the ability to inflate and deflate. But if there is a pressure on the lungs or something blocks the airways, they can’t perform their functions as they should, which may result in atelectasis.
Continue reading to learn more about atelectasis, including its two types: obstructive and non-obstructive atelectasis.
Causes of Obstructive Atelectasis
Causes of atelectasis are different for obstructive and non-obstructive atelectasis. Obstructive atelectasis occurs due to a blocked airway, while non-obstructive atelectasis develops due to pressure from outside the lung.
When airways get blocked, air can’t get to the alveoli, leading to the collapse of the lung and the development of atelectasis. It can have various causes, including:
- Tumor: A growth, not necessarily cancer, may block or narrow the airway.
- Foreign body: Various objects and foreign bodies may block the airway. This cause is more common among children who have inhaled a small object.
- Mucus plug: Mucus plug refers to a build-up of phlegm and sputum in the airways. It is more common in children, during asthma attacks, in people with cystic fibrosis, and after surgery.
Surgeries, particularly procedures that prevent you from coughing, are the most common cause of mucus plug. Moreover, some drugs ordered after surgery may cause weak breathing, making mucus more likely to accumulate in the airways. This is why healthcare specialists perform lung suctioning to get rid of the build-up. But in some cases, the mucus may still accumulate, leading to atelectasis.
Causes of Non-Obstructive Atelectasis
Atelectasis that does not lead to blocked airways is referred to as non-obstructive atelectasis. The causes of this type of atelectasis include surgery, pneumothorax, injury, pleural effusion, chest tumor, lung scarring, and surfactant deficiency.
Surgery
Surgeries that may lead to non-obstructive atelectasis often require from the patients to:
- Stay in bed
- Receive anaesthesia
- Take sedatives or pain medications after the procedure
- Use a machine that supports breathing
These factors may make an individual’s breath weak and less likely to cough, which increases the risk of non-obstructive atelectasis. The inability to breathe deeply and cough may cause parts of the alveoli to collapse. Because of that, it is vital to consult a healthcare professional before the procedure to learn how to reduce the risk of developing atelectasis after the surgery.
Pneumothorax
Pneumothorax, also known as collapsed lung, is a condition sometimes confused with atelectasis. It develops when the air enters the pleural space (space around the lungs). Some of its characteristic symptoms include low blood pressure, anxiety, fatigue, stabbing pain in the chest, and shortness of breath.
Pneumothorax is similar to pleural effusion because it also blocks the airways. However, while fluid is responsible for blockage in pleural effusion, pneumothorax involves a build-up of air. This may lead to lung collapse and the development of atelectasis.
Pleural Effusion
Like pneumothorax, pleural effusion may cause atelectasis due to the build-up in the pleural cavity, a space between two thin membranes surrounding the lungs. These two structures are typically very close to each other but can be separated when the air accumulates in the space between them. As a result, pleural effusion may result in non-obstructive atelectasis and the following symptoms:
- Fever and chills
- Rapid breathing
- Shortness of breath
- Chest pain
- Coughing
Chest Tumor
Chest tumors and growths that put pressure on the lung may cause non-obstructive atelectasis. This happens because tumors can force the air out of the alveoli and deflate them.
Lung Scarring
Also referred to as pulmonary fibrosis, lung scarring is a lung disease that causes respiratory problems such as difficulty breathing and coughing when alveoli become damaged. Lung scarring usually develops due to infections and prolonged exposure to irritants such as smoke or toxins.
Surfactant Deficiency
Alveoli can stay open thanks to a substance called surfactant. If there is not enough of it, alveoli can collapse, potentially leading to atelectasis. Surfactant deficiency is most often observed in infants.
Risk Factors
Some people are more likely to develop atelectasis than others. Factors that increase the risk of this condition include the following:
- Health conditions that make swallowing difficult
- Lung diseases, including asthma, cystic fibrosis, chronic obstructive pulmonary disease (COPD), and bronchiectasis
- Rib fractures and chest injuries which may prevent you from taking deep breaths
- Recent surgery performed in the chest or stomach area
- Medicines that may lead to weak breathing
- Smoking or exposure to tobacco smoke
- Staying in bed for a long time without changing positions
- Injuries that make coughing difficult
- Personal history of lung diseases
- Use of sedatives or opioids
- Cardiopulmonary bypass surgery
- Spinal cord injury
- Muscular dystrophy
- Older age
- Obesity

Signs and Symptoms
The number of issues and severity of symptoms caused by atelectasis vary from person to person. How an individual experiences it depends on how much of the lung is affected, how fast it progresses, and whether complications have developed.
The following symptoms are the most likely to appear in a typical case of atelectasis:
- Fever (high body temperature)
- Coughing
- Shallow and weak breathing
- Production of phlegm or thick mucus
- Chest pain
- Cracking sounds
- Wheezing
- Less chest expansion
Atelectasis that affects a lot of alveoli may cause low blood oxygen and lead to the following symptoms:
- Increased heart rate
- Difficulty breathing
- Rapid breathing
- Blue-colored skin on lips, fingernails, or toenails
- Sharp chest pain triggered by coughing and deep breaths
If pneumonia develops as a complication of atelectasis, you may also experience these health issues:
- Chest pain
- High body tempereture
- Coughing up phlegm

Complications
While atelectasis is not a severe health condition, it may lead to several serious complications. Some of the most often observed include the following:
- Pneumonia: Musus in the collapsed lung increases the risk of infection, so as long as you have atelectasis, you are more likely to develop pneumonia.
- Respiratory failure: In serious cases, atelectasis may lead to respiratory failure. This life-threatening condition occurs when the body does not receive enough oxygen to get it to the blood.
- Low blood oxygen: Known as hypoxemia, low blood oxygen happens when there is a low oxygen level in the blood. Symptoms usually include shortness of breath, confusion, and rapid heart rate.
- Bronchiectasis: Bronchiectasis is a chronic lung condition that occurs due to the widening of the airways.
Diagnosis and Tests
Diagnosis of atelectasis encompasses physical examination, medical history review, lung diseases and surges, and tests. If your doctor suspects a lung condition after the initial assessment, they may order the following tests:
- Ultrasound
- Chest X-ray
- Bronchoscopy
- Computed tomography (CT) scan
- Oximetry or blood gas test
Treatment
In rare cases, atelectasis requires a surgical removal of a small lung area. Healthcare professionals recommend it as a last resort if other treatment strategies are unsuccessful or if there is permanent lung scarring. In other scenarios, treatment usually involves one or a combination of the following therapies and procedures:
- Chest physiotherapy: Chest physiotherapy is a treatment involving the use of vibrations, tapping motions, and vibrating vests to loosen and drain the mucus. Doctors recommend this treatment for obstructive atelectasis and cystic fibrosis.
- Incentive spirometry: During this treatment, patients perform deep breathing exercises through a device to expand the lungs.
- Bronchodilators: Bronchodilators are medicines that help relax the muscles around the airways. They are available in several forms, including inhalers, nebulizers, and tablets.
- Oxygen therapy: Some patients suffering from severe atelectasis may benefit from supplemental oxygen. It provides patients with extra oxygen to breathe in.
- Airway suction: An Airway suction procedure involves removing mucus from the airways with a thin tube.
- Treatment of accompanying conditions: If pneumonia, tumor, or other condition causes atelectasis, it must be treated first.
Prognosis for Atelectasis Patients
Damage caused by atelectasis is usually reversible once the cause is identified and treated. Most people don’t develop severe complications and recover quickly. However, individuals who are struggling with chronic atelectasis may require further treatment and management strategies to relieve the symptoms.
How to Prevent Atelectasis?
It is possible to reduce the risk of lung conditions, including atelectasis, by following a healthy lifestyle and applying good practices for general health. Here are some ideas that would particularly benefit people with atelectasis:
- If you smoke, quitting is crucial for lung health. Smoking damages the lungs and increases the risk of respiratory issues, including atelectasis.
- Drink plenty of fluids to help keep mucus thin and easy to clear from the airways. Proper hydration is essential for overall lung health.
- Change your body position regularly, especially if you are bedridden. This helps prevent areas of the lungs from collapsing due to prolonged pressure.
- Coughing helps clear mucus from the airways, reducing the risk of blockage. If you’ve had surgery or are at risk of atelectasis, your healthcare provider may recommend coughing exercises.
- Perform deep breathing exercises regularly to expand the lungs and prevent shallow breathing. Deep breaths help keep the alveoli open and functioning correctly.
- Take steps to prevent respiratory infections, as they can contribute to atelectasis. Practice good hand hygiene and avoid close contact with individuals who have respiratory infections.
- Follow your healthcare provider’s instructions and recommendations, especially after surgery. This may include specific breathing exercises, medication, or other measures to prevent atelectasis.
It’s important to note that these general recommendations can only help you reduce the risk of developing lung conditions or manage their symptoms better. Still, they can’t replace conventional treatment strategies. Remember to always consult with your healthcare provider for personalized advice based on your medical history and current health status. If you experience symptoms of atelectasis, such as difficulty breathing or chest pain, seek medical as soon as possible.
Key Facts You Should Know
Atelectasis is a lung condition characterized by the partial collapse of alveoli, leading to decreased oxygen levels in the bloodstream and affected breathing. There are two types of atelectasis: obstructive and non-obstructive.
Obstructive atelectasis results from blocked airways, often caused by tumors, foreign bodies, or mucus plugs. Non-obstructive atelectasis occurs due to external pressure on the lung and can result from various causes, including surgery, pneumothorax, pleural effusion, chest tumors, lung scarring, and surfactant deficiency.
Symptoms range from coughing, shallow breathing, and chest pain to more severe issues like fever, rapid heart rate, and low blood oxygen levels. Complications may include pneumonia, respiratory failure, and bronchiectasis.
Treatment options include chest physiotherapy, incentive spirometry, bronchodilators, oxygen therapy, airway suction, and addressing underlying conditions like pneumonia or tumors. Surgical intervention is rare and considered a last resort.
Sources
- MedlinePlus. (2022). Atelectasis.
https://medlineplus.gov/ency/article/000065.htm - NIH. (2023). Atelectasis.
https://www.ncbi.nlm.nih.gov/books/NBK545316/ - Loyola University Chicago. Atelectasis.
https://www.meddean.luc.edu/lumen/meded/medicine/pulmonar/cxr/atelect.htm - Oxford Academic. (2013). Pulmonary atelectasis in anaesthesia and critical care.
https://academic.oup.com/bjaed/article/14/5/236/286828 - Northwestern Medicine. Symptoms of Atelectasis and Pneumothorax.
https://www.nm.org/conditions-and-care-areas/pulmonary/atelectasis-and-pneumothorax/symptoms
- Atelectasis: What Is, Causes, Symptoms, Treatment, and Prevention
- What Is Atelectasis?
- Causes of Obstructive Atelectasis
- Causes of Non-Obstructive Atelectasis
- Risk Factors
- Signs and Symptoms
- Diagnosis and Tests
- Treatment
- Prognosis for Atelectasis Patients
- How to Prevent Atelectasis?
- Key Facts You Should Know