Specialists categorized antidepressants as psychotropic medications – they are instrumental in the management of diverse mental health conditions, including but not restricted to depression and affective disorders. They are also indicated for the treatment of conditions such as obsessive-compulsive disorder, social phobias, panic disorders, anxiety-related depressive disorders, and post-traumatic stress disorder. Furthermore, individuals contending with neurasthenia and chronic neuropathic pain may also benefit from antidepressant therapy.
Types
Due to their chemical structure, we can divide antidepressants into two major groups:
- Tricyclic antidepressants (TCAs) – these are first-generation drugs discovered in the 1950s, now less frequently used. Non-selective type, which means that they affect the concentration of not only serotonin and norepinephrine but also other neurotransmitters. They are highly effective, but at the same time, they are least tolerated by the body and have several side effects (they may contribute to the development of glaucoma, heart disease, and prostatic hypertrophy, among others). This group includes tricyclic norepinephrine (NA) and serotonin (5-HT) reuptake inhibitors and monoamine oxidase inhibitors (MAOIs).
- Drugs with two-ring, four-ring, and other structures – these are second-generation drugs, the most modern type of antidepressant. Belong to them: non-receptive norepinephrine and serotonin reuptake inhibitors (SNRIs), selective serotonin uptake inhibitors (SSRIs), and selective norepinephrine uptake inhibitors (NRIs).
Below, we will take a closer look at some of them.
Tricyclic Antidepressants
Tricyclic antidepressants (TCAs) were first introduced in the 1950s and are primarily employed to treat endogenous depression. Additionally, they may be prescribed to alleviate symptoms of panic disorders, obsessive-compulsive disorders, and psychogenic pain. However, it is noteworthy that TCAs are known to cause various side effects.
Although severe complications are rare, non-compliance with contraindications and instructions may lead to severe anxiety, anxiety, psychomotor agitation, exacerbation of psychotic symptoms in the course of schizophrenia, mania, seizures, and muscle tremors.
Tricyclic drugs can also significantly impact the circulatory system, causing a drop in blood pressure, increased heart rate, and, less frequently, cardiac arrhythmias and decreased myocardial contractility. Therefore, it is advisable to avoid prescribing antidepressants of this type to patients with circulatory system dysfunction, particularly those with cardiac arrhythmias.
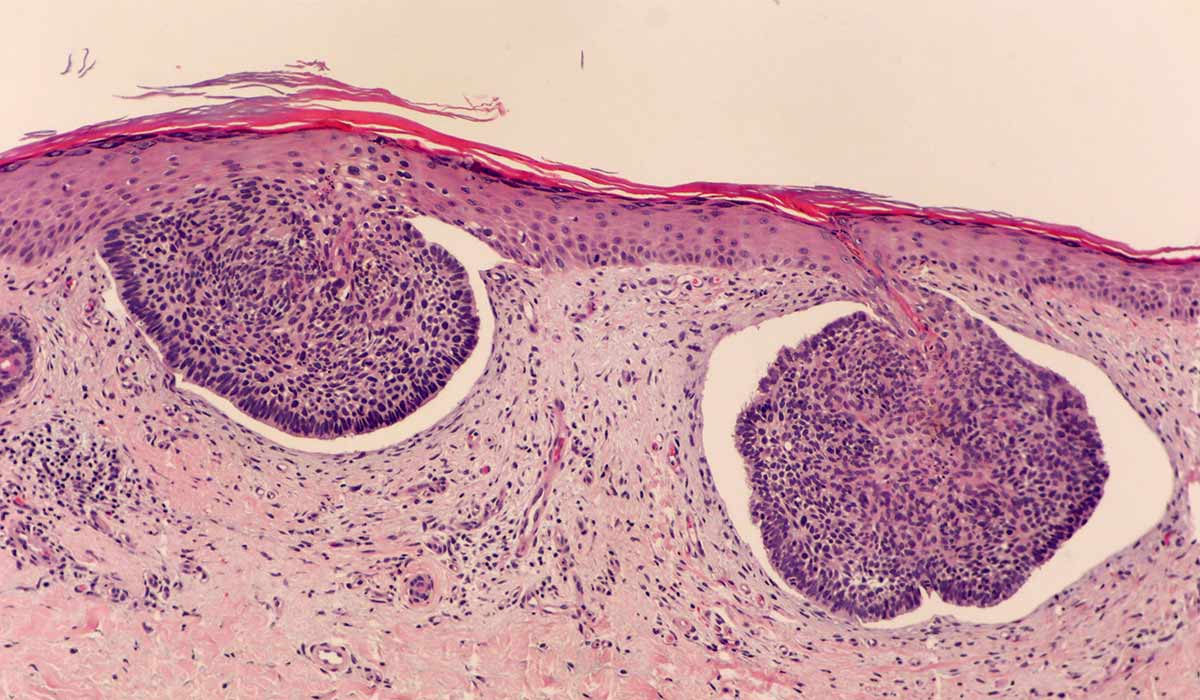
Selective Serotonin Reuptake Inhibitors
Selective serotonin reuptake inhibitors (SSRIs) are a type of second-generation antidepressant that are widely used today. Research and clinical observations have shown that SSRIs are generally better tolerated, safer, and have a narrower range of contraindications than classic tricyclic antidepressants (TCAs).
SSRIs are effective for treating various depressive disorders, especially recurrent disorders, depression accompanying bipolar disorder, and depression at any age. They are also commonly used to treat obsessive-compulsive disorders and emotional disorders such as social phobia, panic disorder, post-traumatic stress, and bulimia.
While the effectiveness of SSRIs is similar to that of TCA, the prevailing opinion among some psychiatrists is that SSRIs are better for mild and moderate depression. In the case of severe depression of the melancholic type combined with additional psychotic symptoms, TCA treatment is indicated. If TCA treatment is ineffective, SSRIs may be used as an alternative.
There are only a few contraindications to SSRI treatment, including breastfeeding, Parkinson’s disease, epilepsy, and liver and kidney failure. Caution should be taken with individuals who have diabetes, circulatory system dysfunction, glaucoma, or prostatic hypertrophy.
Effects
Depression can be explained simply as a chemical imbalance or a serotonin deficiency. Unfortunately, it is more complicated because researchers still haven’t discovered what causes this condition or how antidepressants enhance the signs.
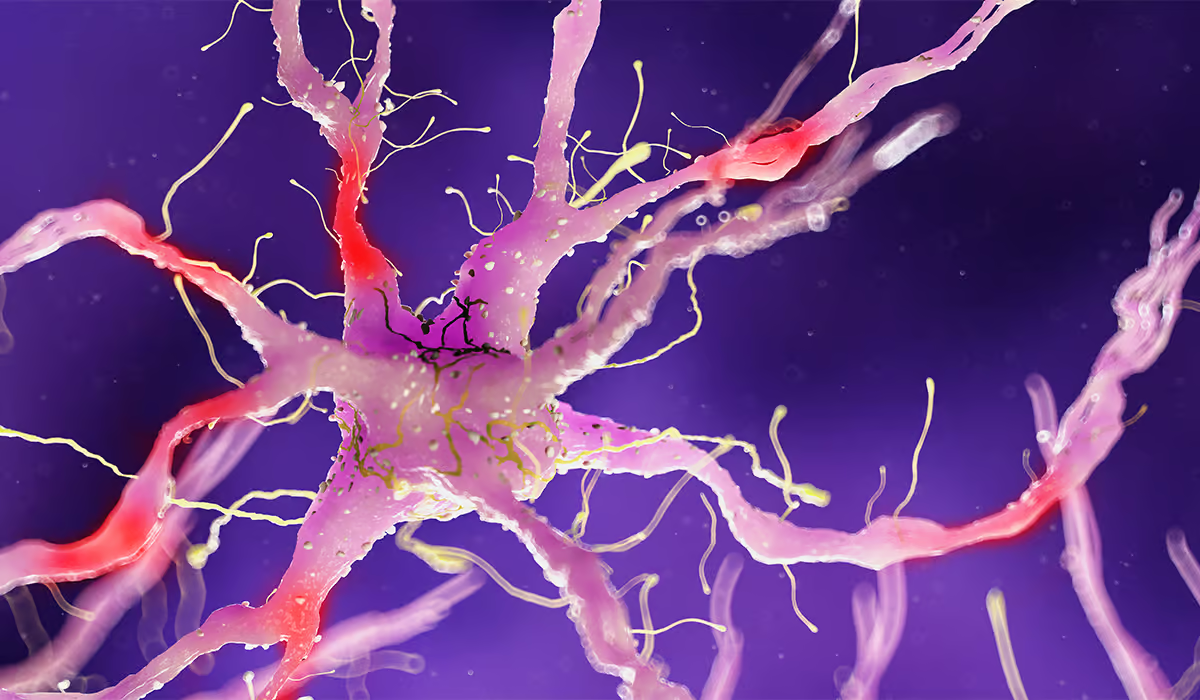
Neurotransmitters
With that stated, many specialists think that the advantages of antidepressants arise from how they influence specific brain circuits and neurotransmitters. Those are chemicals that transport signals from one nerve cell to another. For example, we distinguished serotonin, and norepinephrine. In different forms, various antidepressants impact how these neurotransmitters act.
Reuptake Inhibitors
Let’s look at one of the antidepressant types, reuptake inhibitors. Reuptake is a procedure in which neurotransmitters are reabsorbed back into nerve cells in the brain after they are released to transmit messages between nerve cells. A reuptake inhibitor stops this process. Rather than being reabsorbed, the chemicals stay in the synapse (it is a gap between the nerves). Keeping levels of the neurotransmitters more elevated can enhance transmission between the nerve cells and support circuits in the brain that help to regulate mood.
However, there is a possibility that antidepressants have other unidentified results and that their advantages don’t concern neurotransmitter levels.
When taking an antidepressant, be patient. Some individuals begin therapy and anticipate that it will work right away. But that’s not how they work – they can take weeks or months to gain their complete effect.
Addictiveness
It is commonly believed that antidepressants can be mentally and physically addictive. As psychiatrists emphasize, this is not true. Patients often confuse addiction with withdrawal symptoms (withdrawal syndrome). These symptoms appear when the patient suddenly stops taking the drug or significantly reduces its dose without consulting a doctor.
A side effect of this is a sudden imbalance in the level of neurotransmitters in the brain, which translates into severe mood swings. The patient experiences the following symptoms:
- Sudden deterioration of well-being
- Manic or euphoric states (not that often)
- Anxiety, irritability, or crying spells
- Abdominal pain, nausea, vomiting, and diarrhea
- Sleep disorders psychomotor disorders (excessive excitability or slowness of movement, muscle tremors, and deterioration of vision)
- Muscle pain, tingling, or numbness of the skin
- Hypersensitivity to light
- Increased sweating
Gradually reducing doses under medical supervision reduces the risk of withdrawal symptoms.
In rare cases, withdrawal syndrome may result in a recurrence of depression, requiring resumption of therapy.

Side Effects of Antidepressants
The use of antidepressants is often the subject of concern among patients. Every person responds to medications differently, but some side effects are standard. These are:
- Nausea
- Gaining weight
- Diarrhea
- Constipation
- Problem sleeping
- Dry mouth
- Blurred vision
- Dizziness
- Headache
- Sexual issues
- Anxiety
- Exhaustion
- Tremors
- More sweating than usual
The patient can have many, a few, or none of these. Moreover, those manifestations of using antidepressants may go away a few weeks after the beginning of the treatment.
Side effects may occur when the drug has been incorrectly selected or dosed.
Lesser-Known Side Effects
Some other side effects from antidepressants aren’t debated as frequently. However, they’re still significant to look out for. They can be:
- Lower alcohol tolerance
- Bleeding
- Lower sodium levels
Hyponatremia
Observe if there is a manifestation of hyponatremia when you’re adapting to a new medicament. These include:
- Headaches
- Nausea
- Vomiting
- Drowsiness
- Confusion
- Fatigue
- Crankiness
- Restlessness
- Muscle cramps or spasms
- General body weakness
- Seizures
Consult specialists if you detect these signs.
Withdrawal Symptoms
The withdrawal symptoms that occur following their sudden discontinuation are a result of the drugs’ effect on various types of neurotransmitter pathways in the brain. Deprived of the previously supplied substance, these pathways must adapt to this state again. However, they are not accompanied by a craving for the substance and an irresistible, difficult-to-control desire to take it again, which are characteristic of the withdrawal syndrome that occurs after stopping stimulants.
It is worth noting that while it takes at least 2-3 weeks to improve mood after taking antidepressants, an anxiety reduction is observed at the beginning of treatment. This is particularly important in patients who are experiencing suicidal thoughts, as it may result in a greater propensity to act on them. During this time, loved ones should remain vigilant, and in cases of high suicide risk, it is recommended to initiate treatment under the supervision of specialists in a hospital setting.
General Principles of Treatment
One of the most critical aspects of depression treatment is establishing good cooperation with the specialist. Patients should not make independent decisions regarding treatment modifications but should inform their doctor of all symptoms and concerns, enabling the physician to choose the optimal treatment.
When selecting medications for patients, psychiatrists follow several fundamental principles, including using the lowest effective dose of the drug. This is because the chance of side effects increases with higher doses, and therapy costs also increase.
How Long Should You Take Them?
Assessing the effectiveness of treatment is not recommended until at least 1-2 weeks after initiation because antidepressants affect complex cellular processes that cannot be modified immediately. If the patient does not experience improvement after 6-8 weeks of using the maximum dose of a given drug, specialists typically recommend changing the drug to another from the same group. If this does not work, they may prescribe a drug from another group.
After the first episode of depression, patients are encouraged to take medications for at least six months following symptom resolution. In the event of a subsequent episode of depression, treatment should continue for a more extended period, up to 2 years after symptom disappearance. If a third episode occurs, the specialist may consider permanent use of the drug.
Who Can Help?
Determining the most suitable antidepressant for a patient necessitates a comprehensive interview conducted by a physician. The physician selects the most appropriate medication for the patient based on the depressive symptoms they are experiencing.

Things to Remember When Choosing The Right Antidepressant
There are many kinds of medicament available that work in narrowly various ways and have diverse side effects. When choosing an appropriate antidepressant the specialist will consider:
- The symptoms – may differ, and one medicament can reduce specific signs better. For example, if you experience issues with sleeping, an antidepressant that induces calmness or sleepiness can be a suitable choice.
- Potential side effects – they also differ from one antidepressant to another and from person to person. Bothersome consequences may make it challenging to continue pharmacotherapy. Consult your doctor about potential significant side effects.
- Interaction with other medications – some antidepressants may induce harmful responses when mixed with other medications.
- Pregnancy or breastfeeding – a decision to take antidepressants while being pregnant or breastfeeding can be based on the ratio between disadvantages and advantages. In general, the risk of birth defects and other issues is low. Nevertheless, specific medicaments are not used during pregnancy or breastfeeding.
- Other health conditions – some antidepressants can induce issues if the patient has particular mental or physical health conditions. On the other hand, particular medicaments can help manage other diseases along with depression.
- Cost and health insurance coverage – some medications may be pricey, so it is better to ask if there is a generic version available and consult its efficacy. Moreover, the patient should find out whether their health insurance covers buying antidepressants and if there are any restrictions on which ones are covered.
Sources
- Antidepressants. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK538182/ - Tricyclic Antidepressants. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK557791/ - Selective Serotonin Reuptake Inhibitors. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK554406/ - How antidepressant drugs act: A primer on neuroplasticity as the eventual mediator of antidepressant efficacy. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3025168/ - Reuptake inhibitor. APA.
https://dictionary.apa.org/reuptake-inhibitor - Antidepressants, withdrawal, and addiction; where are we now?. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7613097/ - Depression: How effective are antidepressants?. NIH.
https://www.ncbi.nlm.nih.gov/books/NBK361016/ - Estimating Risk of Antidepressant Withdrawal from a Review of Published Data. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC9911477/ - Choosing an antidepressant. NIH.
https://pubmed.ncbi.nlm.nih.gov/33664544/ - Understanding Side Effects of Antidepressants: Large-scale Longitudinal Study on Social Media Data. NIH.
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8077932/ - Antidepressants and the risk of hyponatremia: a class-by-class review of literature. NIH.
https://pubmed.ncbi.nlm.nih.gov/25262043/